Piriformis Syndrome, often abbreviated as PS, is a condition that occurs when the piriformis muscle irritates or compresses the sciatic nerve. This can lead to pain, numbness, and tingling sensations in the buttocks and down the leg. Although it is not as widely recognized as other causes of sciatica, Piriformis Syndrome can significantly impact an individual’s quality of life if left untreated. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition.

Understanding the Piriformis Muscle
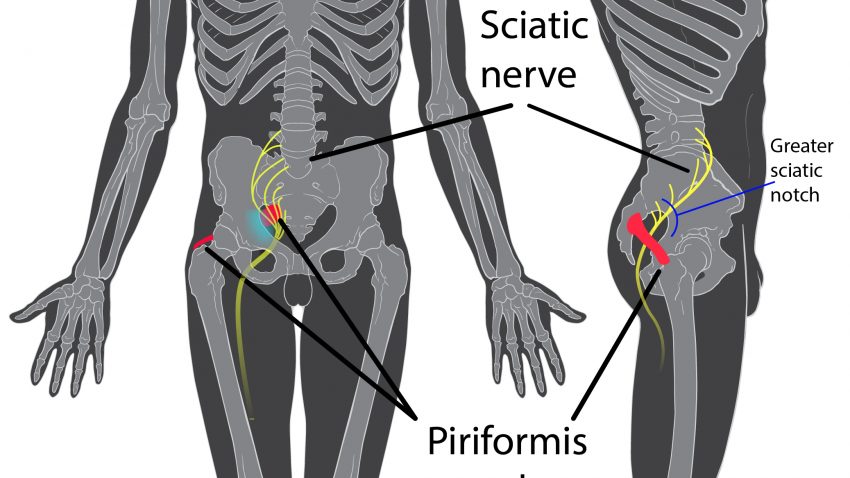
The piriformis muscle is a small but important muscle located deep within the buttocks. It connects the lower spine to the upper surface of the thigh bone and plays a crucial role in hip rotation and stability. When this muscle becomes tight or inflamed, it can press against the sciatic nerve, which runs directly beneath or sometimes through the muscle. This compression is what leads to the symptoms associated with Piriformis Syndrome.
Anatomy of the Piriformis Muscle
- Location: The piriformis muscle is situated in the gluteal region, near the base of the spine.
- Function: It helps rotate the hip outward and stabilizes the pelvis during movement.
- Relation to the Sciatic Nerve: In some individuals, the sciatic nerve passes through the piriformis muscle, making them more susceptible to irritation.
Causes of Piriformis Syndrome
There are several factors that can contribute to the development of Piriformis Syndrome. These include both physical and lifestyle-related causes. Understanding these triggers can help individuals take preventive measures and seek appropriate treatment.
Injury or Trauma
Direct injury to the buttock area, such as from a fall or a car accident, can damage the piriformis muscle. This trauma may cause inflammation or spasms, leading to compression of the sciatic nerve.
Prolonged Sitting
Sitting for extended periods, especially on hard surfaces, can put pressure on the piriformis muscle. Over time, this pressure can irritate the muscle and the nearby sciatic nerve, resulting in discomfort.
Overuse or Strain
Repetitive activities that involve the legs, such as running, climbing stairs, or squatting, can strain the piriformis muscle. Athletes and individuals who engage in high-impact sports are particularly at risk.
Anatomical Variations
In some people, the sciatic nerve passes through the piriformis muscle instead of underneath it. This anatomical variation increases the likelihood of nerve compression when the muscle contracts or becomes inflamed.
Symptoms of Piriformis Syndrome
The symptoms of Piriformis Syndrome can vary from person to person, but they typically involve pain and discomfort in the buttocks and legs. Recognizing these symptoms early can aid in timely diagnosis and treatment.
Pain in the Buttocks
One of the hallmark symptoms of Piriformis Syndrome is a dull ache or sharp pain in the buttocks. This pain may worsen when sitting for long periods or engaging in activities that require hip movement.
Radiating Pain Down the Leg
Individuals with this condition often experience pain that radiates down the back of the leg, similar to sciatica. This sensation may be accompanied by a burning or tingling feeling.
Numbness and Tingling
Compression of the sciatic nerve can also cause numbness or a pins-and-needles sensation in the affected leg. These symptoms may come and go depending on the level of irritation.
Muscle Weakness
In severe cases, prolonged nerve compression can lead to weakness in the muscles of the leg. This may affect mobility and make it difficult to perform daily tasks.
Diagnosing Piriformis Syndrome
Diagnosing Piriformis Syndrome can be challenging because its symptoms overlap with other conditions, such as herniated discs or spinal stenosis. A thorough evaluation by a healthcare professional is essential for accurate diagnosis.
Medical History and Physical Examination
A doctor will begin by reviewing the patient’s medical history and conducting a physical examination. During the exam, the doctor may apply pressure to the piriformis muscle to check for tenderness or pain. They may also ask the patient to perform specific movements to assess flexibility and range of motion.
FABER Test
The FABER test (Flexion, ABduction, and External Rotation) is commonly used to diagnose Piriformis Syndrome. The patient lies on their back while the doctor gently moves the affected leg into a bent position. Pain or discomfort during this maneuver may indicate involvement of the piriformis muscle.
Imaging Tests
In some cases, imaging tests such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be ordered. While these tests cannot directly diagnose Piriformis Syndrome, they can rule out other potential causes of sciatic pain, such as herniated discs or arthritis.
Electromyography
Electromyography (EMG) measures the electrical activity of muscles and nerves. This test can help determine whether the sciatic nerve is being compressed and identify the source of the problem.
Treatment Options for Piriformis Syndrome
Treatment for Piriformis Syndrome focuses on relieving pain, reducing inflammation, and restoring normal function to the affected muscle. The approach may vary depending on the severity of the condition and the individual’s response to therapy.
Rest and Activity Modification
For mild cases, resting the affected area and avoiding activities that aggravate the symptoms can provide relief. Modifying daily routines to reduce strain on the piriformis muscle is often recommended.
Physical Therapy
Physical therapy is one of the most effective treatments for Piriformis Syndrome. A therapist can design a personalized exercise program to stretch and strengthen the piriformis muscle and surrounding areas. Common exercises include:
- Piriformis stretches
- Hip flexor stretches
- Core strengthening exercises
Heat and Ice Therapy
Applying heat or ice to the affected area can help alleviate pain and reduce inflammation. Heat therapy relaxes tight muscles, while ice therapy numbs the area and reduces swelling.
Medications
Over-the-counter pain relievers such as ibuprofen or naproxen can help manage pain and inflammation. In more severe cases, a doctor may prescribe muscle relaxants or anti-inflammatory medications.
Injections
Corticosteroid injections may be administered directly into the piriformis muscle to reduce inflammation and relieve nerve compression. In some cases, botulinum toxin (Botox) injections are used to temporarily paralyze the muscle and prevent spasms.
Massage Therapy
Massage therapy can help release tension in the piriformis muscle and improve blood flow to the area. Deep tissue massage techniques are particularly effective for addressing tightness and discomfort.
Surgical Intervention
Surgery is considered a last resort for treating Piriformis Syndrome and is only recommended when all other treatments have failed. The procedure involves releasing or partially removing the piriformis muscle to relieve pressure on the sciatic nerve.
Lifestyle Changes to Prevent Piriformis Syndrome
Making certain lifestyle adjustments can help prevent the recurrence of Piriformis Syndrome. These changes focus on maintaining good posture, staying active, and avoiding behaviors that strain the piriformis muscle.
Ergonomic Adjustments
Using ergonomic chairs and cushions can reduce pressure on the buttocks during prolonged sitting. Taking regular breaks to stand and stretch is also beneficial.
Regular Exercise
Incorporating low-impact exercises such as swimming, walking, or yoga into your routine can strengthen the muscles around the hips and pelvis, reducing the risk of injury.
Proper Lifting Techniques
Learning how to lift objects correctly can prevent unnecessary strain on the piriformis muscle. Always bend at the knees and keep the back straight when lifting heavy items.
Weight Management
Maintaining a healthy weight reduces stress on the muscles and joints, lowering the likelihood of developing musculoskeletal issues like Piriformis Syndrome.