A peritonsillar abscess, often abbreviated as PTA, is a serious medical condition that involves the collection of pus in the tissues surrounding the tonsils. This infection can cause significant discomfort and may lead to complications if not treated promptly. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition to provide a comprehensive understanding of how it affects individuals.
What is a Peritonsillar Abscess?
A peritonsillar abscess occurs when an infection spreads beyond the tonsils into the surrounding soft tissues. It is most commonly seen in young adults but can affect individuals of all ages. The condition typically arises as a complication of untreated or inadequately treated tonsillitis, which is an inflammation of the tonsils caused by bacterial or viral infections.
Causes of a Peritonsillar Abscess
The development of a peritonsillar abscess is closely linked to infections of the throat and tonsils. Below are the primary causes:
- Bacterial Infections: The most common bacteria responsible for causing this condition are Streptococcus pyogenes, which is also known for causing strep throat. Other bacteria, such as Staphylococcus aureus and anaerobic bacteria, can also contribute to the formation of an abscess.
- Viral Infections: Although less common, certain viruses can weaken the immune system and make the throat more susceptible to secondary bacterial infections, leading to abscess formation.
- Tonsillitis: Chronic or recurrent tonsillitis increases the risk of developing a peritonsillar abscess. When the infection spreads from the tonsils to nearby tissues, an abscess may form.
- Poor Oral Hygiene: Poor dental care and oral hygiene can create an environment where bacteria thrive, increasing the likelihood of infections that may lead to abscess formation.
- Weakened Immune System: Individuals with weakened immune systems, such as those with diabetes or HIV, are at a higher risk of developing severe infections, including peritonsillar abscesses.
Symptoms of a Peritonsillar Abscess
The symptoms of a peritonsillar abscess can vary depending on the severity of the infection, but they generally include the following:
- Severe Sore Throat: One of the hallmark symptoms is a severe sore throat that is often worse on one side. The pain may radiate to the ear on the affected side.
- Fever and Chills: A high fever accompanied by chills is a common sign of infection.
- Difficulty Swallowing: Patients may experience significant difficulty swallowing, which can lead to dehydration if fluids are not consumed adequately.
- Muffled Voice: The swelling caused by the abscess can affect the vocal cords, resulting in a muffled or “hot potato” voice.
- Swollen Lymph Nodes: The lymph nodes in the neck may become swollen and tender to the touch.
- Drooling: Due to difficulty swallowing, some patients may drool saliva instead of swallowing it.
- Trismus: Trismus refers to difficulty opening the mouth fully, which occurs due to inflammation of the muscles around the jaw.
- Halitosis: Bad breath is another symptom that may be present due to the presence of pus and bacteria in the throat.
Diagnosis of a Peritonsillar Abscess
Diagnosing a peritonsillar abscess requires a thorough clinical evaluation by a healthcare professional. The diagnostic process typically includes the following steps:
Physical Examination
A doctor will begin by examining the patient’s throat using a light and tongue depressor. They will look for signs of swelling, redness, and asymmetry in the tonsillar area. The presence of a bulging mass near the tonsils is a strong indicator of an abscess.
Medical History
The healthcare provider will ask about the patient’s symptoms, their duration, and any previous history of tonsillitis or throat infections. This information helps establish a clearer picture of the underlying cause.
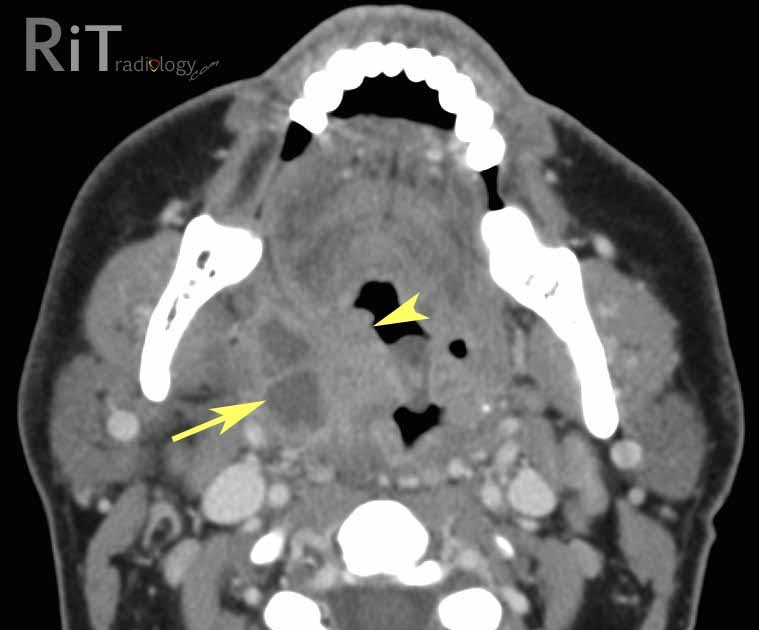
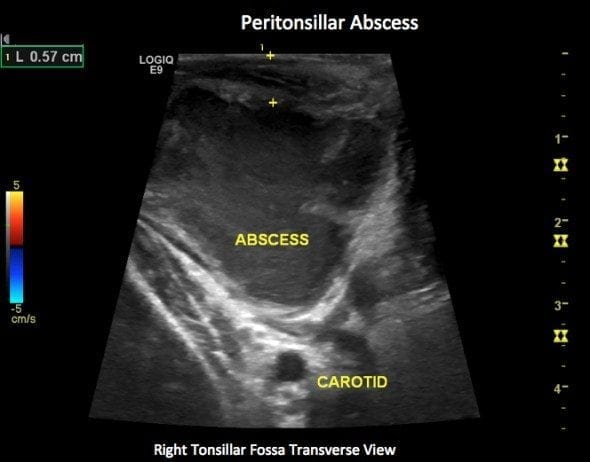
Imaging Tests
In some cases, imaging tests may be necessary to confirm the diagnosis or rule out other conditions. These tests may include:
- Ultrasound: An ultrasound of the neck can help identify fluid collections and differentiate between an abscess and other types of swelling.
- Computed Tomography (CT) Scan: A CT scan provides detailed images of the throat and surrounding structures, helping to pinpoint the exact location and size of the abscess.
Laboratory Tests
Blood tests may be performed to check for elevated white blood cell counts, which indicate an active infection. Additionally, a throat swab may be taken to identify the specific bacteria causing the infection.
Treatment Options for a Peritonsillar Abscess
Treatment for a peritonsillar abscess focuses on draining the abscess and addressing the underlying infection. The approach may vary depending on the severity of the condition and the patient’s overall health.
Antibiotics
Antibiotics are a critical component of treatment for a peritonsillar abscess. Broad-spectrum antibiotics are typically prescribed initially to target a wide range of bacteria. Once the specific bacteria are identified through laboratory tests, the antibiotic regimen may be adjusted accordingly. Commonly used antibiotics include penicillin, clindamycin, and metronidazole.
Drainage Procedures
Draining the abscess is essential to relieve symptoms and prevent complications. There are two primary methods for drainage:
- Needle Aspiration: A needle is inserted into the abscess to withdraw the pus. This procedure is minimally invasive and can be performed in an outpatient setting.
- Incision and Drainage: In more severe cases, a small incision may be made to allow the pus to drain. This procedure is usually performed under local anesthesia.
Tonsillectomy
In recurrent cases of peritonsillar abscess or when conservative treatments fail, a tonsillectomy may be recommended. This surgical procedure involves the removal of the tonsils and is often considered a long-term solution to prevent future abscesses.
Pain Management
Pain relief is an important aspect of treatment, as patients often experience significant discomfort. Over-the-counter pain medications, such as acetaminophen or ibuprofen, may be recommended. In severe cases, stronger prescription pain relievers may be necessary.
Hydration and Rest
Patients are encouraged to stay hydrated by drinking plenty of fluids, even if swallowing is difficult. Adequate rest is also crucial to support the body’s healing process.
Potential Complications
If left untreated, a peritonsillar abscess can lead to serious complications, including:
- Airway Obstruction: Severe swelling can block the airway, making it difficult to breathe.
- Spread of Infection: The infection can spread to nearby areas, such as the neck or chest, leading to conditions like mediastinitis or sepsis.
- Rupture of the Abscess: If the abscess ruptures, it can cause further complications, including aspiration of pus into the lungs.
Prevention Tips
While it may not always be possible to prevent a peritonsillar abscess, certain measures can reduce the risk:
- Good Oral Hygiene: Regular brushing, flossing, and dental check-ups can help prevent infections in the mouth and throat.
- Treating Tonsillitis Promptly: Early treatment of tonsillitis with antibiotics, when appropriate, can prevent the progression to an abscess.
- Avoiding Smoking: Smoking weakens the immune system and irritates the throat, increasing susceptibility to infections.
- Strengthening the Immune System: Eating a balanced diet, exercising regularly, and getting enough sleep can help boost immunity.
When to Seek Medical Attention
Individuals experiencing symptoms of a peritonsillar abscess should seek medical attention promptly. Warning signs that require immediate care include:
- Difficulty breathing or swallowing
- High fever that does not improve with medication
- Severe pain that interferes with daily activities
- Swelling that worsens over time