Peripheral neuropathy, often referred to as PN, is a condition that affects the peripheral nervous system, which is responsible for transmitting signals between the brain, spinal cord, and the rest of the body. This disorder can result in pain, weakness, numbness, and other complications due to damage or dysfunction of the nerves. Understanding the underlying causes, recognizing the symptoms, undergoing proper diagnosis, and exploring treatment options are essential steps in managing this condition effectively.
Understanding Peripheral Neuropathy
Peripheral neuropathy occurs when there is damage to the peripheral nerves. These nerves extend from the central nervous system to various parts of the body, including the hands, feet, arms, and legs. When these nerves are damaged, they may send incorrect signals to the brain, leading to discomfort, loss of sensation, or even paralysis in severe cases.
How Peripheral Neuropathy Affects the Body
The peripheral nervous system plays a vital role in controlling movement, relaying sensory information, and regulating involuntary functions like heart rate and digestion. When peripheral neuropathy develops, it disrupts these processes. For example:
- Sensory nerves may fail to transmit sensations such as touch, temperature, or pain accurately.
- Motor nerves may cause muscle weakness or difficulty in coordination.
- Autonomic nerves may lead to problems with blood pressure, digestion, or bladder control.
Causes of Peripheral Neuropathy
There are numerous potential causes of peripheral neuropathy, ranging from systemic diseases to external factors. Identifying the root cause is crucial for effective treatment.
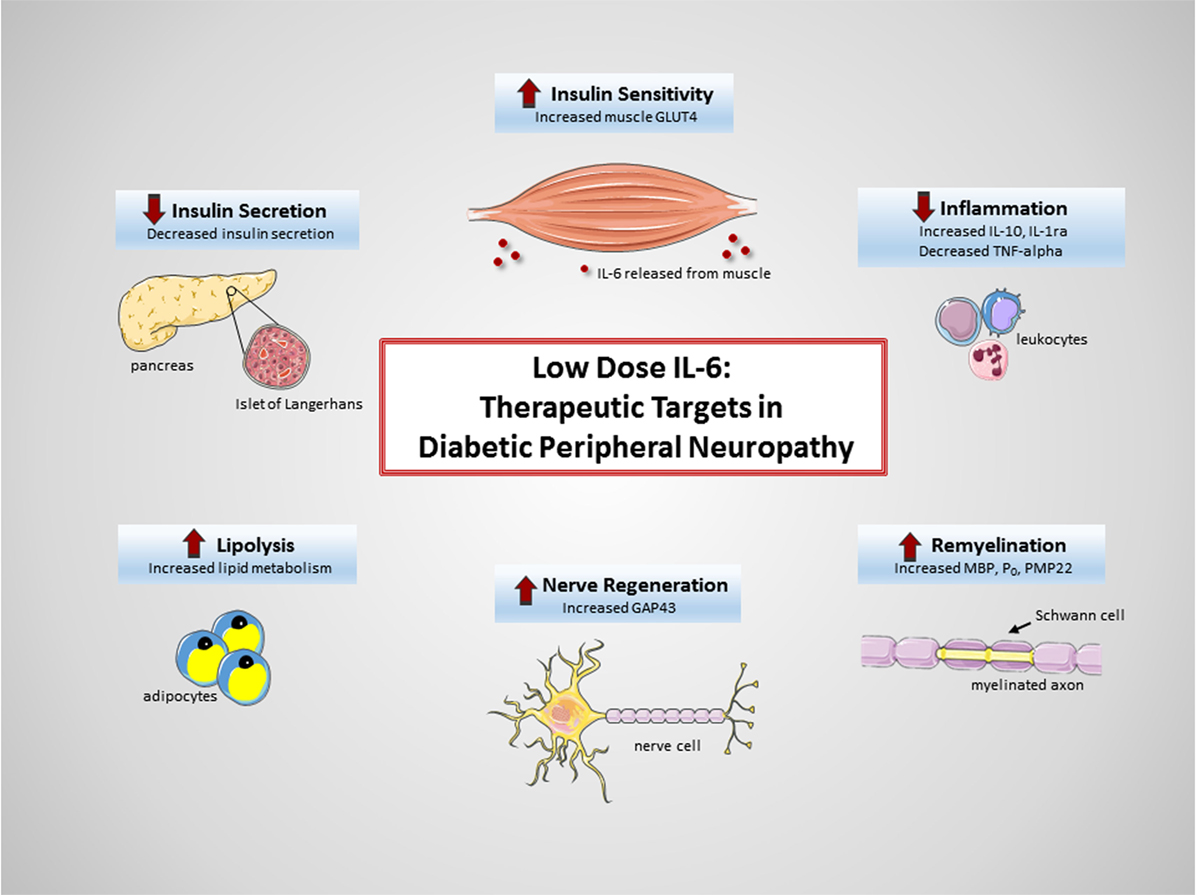
Diabetes
One of the most common causes of peripheral neuropathy is diabetes. High blood sugar levels over time can damage the small blood vessels that supply oxygen and nutrients to the nerves, leading to nerve damage. Diabetic neuropathy often affects the feet and legs first, causing tingling, burning sensations, or numbness.
Autoimmune Disorders
Conditions such as rheumatoid arthritis, lupus, and Guillain-Barre syndrome can trigger an immune response that mistakenly attacks the body’s own nerve tissues. This autoimmune activity can result in inflammation and nerve damage, contributing to peripheral neuropathy.
Infections
Certain infections, including viral and bacterial diseases, can directly attack the nerves or indirectly cause nerve damage through inflammation. Examples include shingles, Lyme disease, hepatitis C, and human immunodeficiency virus.
Trauma or Injury
Physical injuries, such as car accidents, falls, or repetitive stress, can compress, stretch, or sever nerves. This type of trauma often leads to localized nerve damage, resulting in symptoms specific to the affected area.
Toxins and Medications
Exposure to toxins, such as heavy metals or industrial chemicals, can harm the nerves. Additionally, certain medications, particularly those used in chemotherapy, may have neurotoxic effects, leading to peripheral neuropathy as a side effect.
Nutritional Deficiencies
A lack of essential vitamins and minerals, such as vitamin B12, vitamin E, and copper, can impair nerve function. Malnutrition or conditions that interfere with nutrient absorption, like celiac disease or alcoholism, may increase the risk of developing this condition.
Genetic Factors
Some forms of peripheral neuropathy are hereditary, meaning they are passed down through families. Charcot-Marie-Tooth disease is one example of a genetic disorder that causes progressive nerve damage.
Symptoms of Peripheral Neuropathy
The symptoms of peripheral neuropathy vary depending on the type of nerves affected and the severity of the damage. They can range from mild discomfort to debilitating pain.
Sensory Symptoms
Damage to sensory nerves often results in altered sensations. Common symptoms include:
- Tingling or prickling sensations, often described as “pins and needles”
- Burning pain or sharp, shooting pains
- Numbness or reduced ability to feel pain, temperature changes, or touch
- Heightened sensitivity to touch, where even light pressure feels painful
Motor Symptoms
When motor nerves are affected, individuals may experience:
- Muscle weakness or difficulty moving certain parts of the body
- Lack of coordination or balance issues, increasing the risk of falls
- Muscle cramps, twitching, or paralysis in severe cases
Autonomic Symptoms
Dysfunction of autonomic nerves can lead to a wide range of symptoms, including:
- Dizziness or lightheadedness due to changes in blood pressure
- Excessive sweating or inability to sweat
- Digestive issues such as nausea, vomiting, diarrhea, or constipation
- Urinary problems, such as difficulty emptying the bladder completely
Diagnosing Peripheral Neuropathy
Diagnosing peripheral neuropathy involves a combination of medical history evaluation, physical examinations, and diagnostic tests. The goal is to identify the underlying cause and assess the extent of nerve damage.
Medical History and Physical Examination
A healthcare provider will begin by reviewing the patient’s medical history, including any existing conditions, medications, and lifestyle factors. During the physical examination, they will check for signs of nerve damage, such as muscle weakness, loss of reflexes, or changes in sensation.
Diagnostic Tests
Several tests may be conducted to confirm the diagnosis and determine the cause of peripheral neuropathy:
- Nerve Conduction Studies: These tests measure how quickly electrical signals travel through the nerves. Slower-than-normal speeds indicate nerve damage.
- Electromyography: This test evaluates the electrical activity in muscles and helps identify whether muscle weakness is due to nerve damage.
- Blood Tests: Blood samples can reveal underlying conditions, such as diabetes, vitamin deficiencies, or autoimmune disorders.
- Imaging Tests: Techniques like magnetic resonance imaging or computed tomography scans may be used to rule out tumors, herniated discs, or other structural abnormalities that could compress the nerves.
- Nerve Biopsy: In some cases, a small sample of nerve tissue may be removed and examined under a microscope to identify the cause of nerve damage.
Treatment Options for Peripheral Neuropathy
While peripheral neuropathy cannot always be cured, its symptoms can often be managed effectively. Treatment focuses on addressing the underlying cause, relieving symptoms, and improving quality of life.
Managing Underlying Conditions
If peripheral neuropathy is caused by an underlying condition, treating that condition is the first step. For example:
- Controlling blood sugar levels in people with diabetes can slow the progression of nerve damage.
- Medications or therapies for autoimmune disorders may reduce inflammation and prevent further nerve damage.
- Addressing nutritional deficiencies through dietary changes or supplements can help restore nerve health.
Medications for Symptom Relief
Several medications are available to alleviate the discomfort associated with peripheral neuropathy:
- Pain relievers, such as over-the-counter acetaminophen or prescription opioids, may be used for severe pain.
- Antidepressants, such as amitriptyline or duloxetine, can help manage chronic pain by altering the way the brain perceives pain signals.
- Anticonvulsant drugs, such as gabapentin or pregabalin, are often prescribed to reduce nerve-related pain.
- Topical treatments, such as lidocaine patches or capsaicin cream, can provide localized relief.
Therapies and Procedures
In addition to medications, various therapies and procedures may be recommended:
- Physical Therapy: Exercises designed to improve strength, flexibility, and balance can help counteract muscle weakness and prevent falls.
- Occupational Therapy: This therapy teaches patients adaptive techniques to perform daily activities despite limitations caused by peripheral neuropathy.
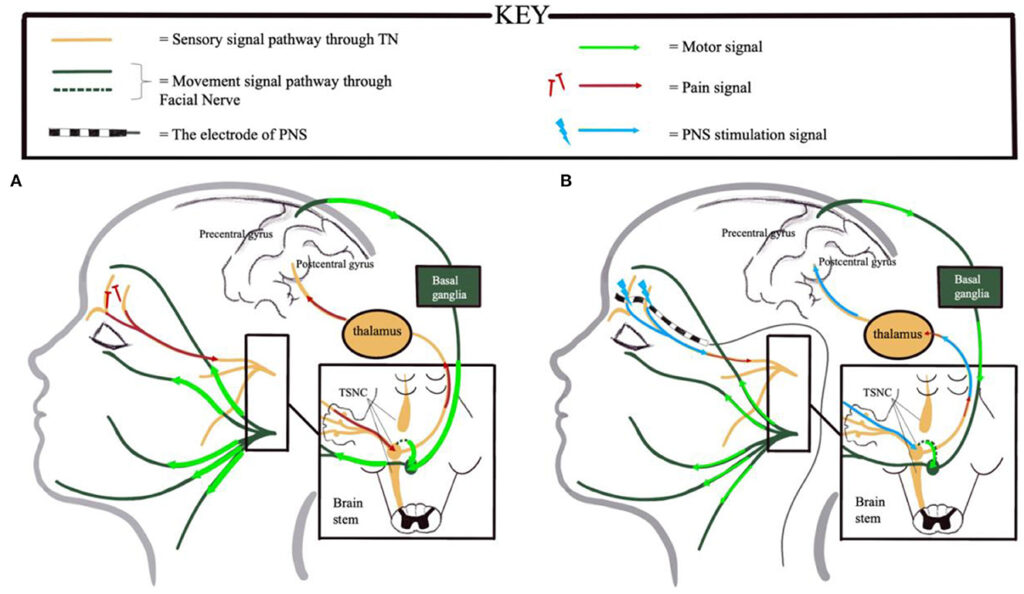
- Transcutaneous Electrical Nerve Stimulation: This non-invasive procedure uses low-voltage electrical currents to relieve pain.
- Plasma Exchange or Intravenous Immune Globulin: These treatments suppress immune system activity and are sometimes used for autoimmune-related neuropathies.
Lifestyle Modifications
Making certain lifestyle changes can also play a significant role in managing peripheral neuropathy:
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports overall nerve health.
- Exercise: Regular physical activity improves circulation, reduces stress, and enhances muscle strength.
- Avoiding Alcohol and Toxins: Limiting alcohol consumption and avoiding exposure to harmful substances can prevent further nerve damage.
- Proper Foot Care: Individuals with peripheral neuropathy should inspect their feet daily for cuts, blisters, or sores, as reduced sensation increases the risk of unnoticed injuries.
Alternative and Complementary Therapies
Some individuals find relief through alternative approaches, though these should complement rather than replace conventional treatments:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to stimulate nerve function and reduce pain.
- Massage Therapy: Massaging the affected areas can improve circulation and relax tense muscles.
- Mind-Body Practices: Techniques such as yoga, meditation, and tai chi can reduce stress and promote relaxation, which may indirectly ease neuropathic symptoms.