Peripheral Arterial Disease, commonly referred to as PAD, is a condition that affects millions of people worldwide. It occurs when the arteries in the legs become narrowed or blocked due to the buildup of fatty deposits, leading to reduced blood flow. This guide aims to provide a comprehensive understanding of this condition, its causes, symptoms, diagnosis, treatment options, and lifestyle changes that can help manage it effectively.
Understanding the Condition
Peripheral Arterial Disease is a circulatory problem where narrowed arteries reduce blood flow to the limbs, most commonly the legs. When the arteries are blocked or narrowed, the limbs do not receive enough oxygen-rich blood, which can cause pain and other complications. The condition is often a sign of widespread accumulation of fatty deposits in the arteries, known as atherosclerosis, which can also affect the heart and brain.
How Does the Disease Develop?
The development of this disease begins with damage to the inner layers of the arteries. Factors such as smoking, high cholesterol levels, high blood pressure, diabetes, and obesity contribute to this damage. Over time, fats, cholesterol, and other substances build up on the walls of the arteries, forming plaques. These plaques harden and narrow the arteries, restricting blood flow.
Risk Factors for Developing the Condition
- Age: People over the age of 50 are at a higher risk.
- Smoking: Smoking is one of the most significant risk factors.
- Diabetes: High blood sugar levels increase the risk.
- High Blood Pressure: Uncontrolled blood pressure can damage artery walls.
- High Cholesterol: Elevated cholesterol levels contribute to plaque formation.
- Obesity: Excess weight puts additional strain on the circulatory system.
- Family History: A family history of circulatory problems increases risk.
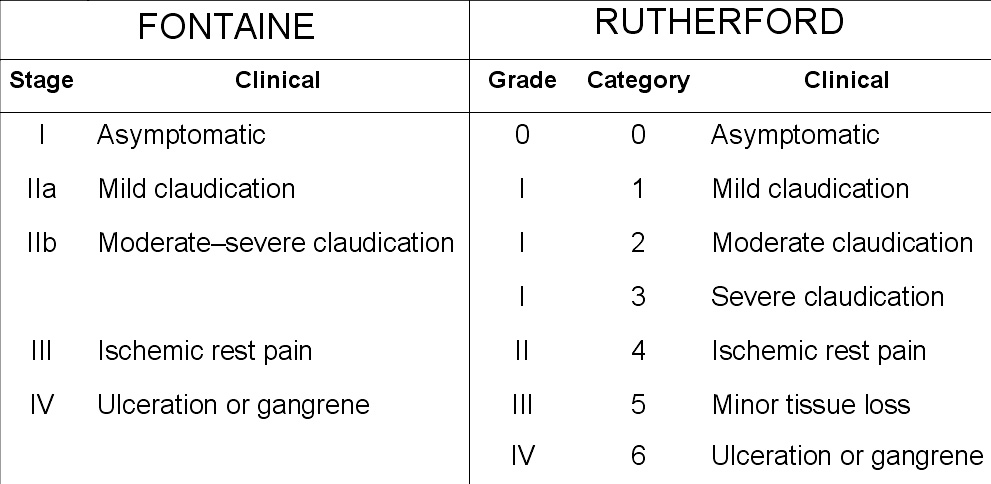
Symptoms of Peripheral Arterial Disease
Many individuals with this condition may not experience any symptoms initially. However, as the disease progresses, certain signs may become apparent. Recognizing these symptoms early can help prevent further complications.
Common Symptoms
- Painful Cramping: Pain in the legs or hips during activities like walking or climbing stairs, which subsides with rest.
- Coldness in the Lower Leg or Foot: One leg may feel colder than the other.
- Changes in Skin Color: The skin on the legs may appear pale or bluish.
- Slow-Healing Sores: Wounds on the feet or legs take longer to heal.
- Hair Loss: Hair loss on the legs or slower hair growth.
- Weak Pulse: A weak or absent pulse in the legs or feet.
When to Seek Medical Attention
If you experience persistent leg pain, especially during physical activity, or notice any of the above symptoms, it is important to consult a healthcare provider. Early diagnosis and treatment can prevent the progression of the disease and reduce the risk of complications such as infections, ulcers, or even amputation.
Diagnosing the Condition
Diagnosing this circulatory condition involves a combination of physical examinations, medical history reviews, and specialized tests. Healthcare providers use these methods to assess blood flow and identify blockages in the arteries.
Physical Examination
A healthcare provider will begin by examining the legs for signs of poor circulation, such as coldness, discoloration, or weak pulses. They may also check for wounds or sores that are slow to heal.
Medical History Review
Understanding your medical history is crucial. The provider will ask about risk factors such as smoking, diabetes, high blood pressure, and family history of circulatory problems.
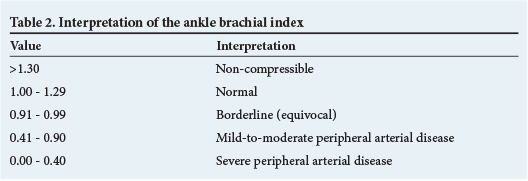
Diagnostic Tests
- Ankle-Brachial Index: This test compares the blood pressure in the ankle to that in the arm to determine how well blood is flowing in the legs.
- Doppler Ultrasound: This imaging test uses sound waves to evaluate blood flow through the arteries.
- Magnetic Resonance Angiography: This advanced imaging technique provides detailed images of the arteries.
- Angiography: A contrast dye is injected into the arteries to visualize blockages using X-rays.
Treatment Options
Treatment for this condition focuses on managing symptoms, improving mobility, and preventing further complications. Depending on the severity of the disease, treatment may involve lifestyle changes, medications, or surgical procedures.
Lifestyle Changes
Adopting healthier habits is often the first step in managing this condition. These changes can improve blood flow and reduce the risk of complications.
- Quitting Smoking: Smoking cessation is critical for slowing the progression of the disease.
- Regular Exercise: Walking programs can improve circulation and reduce symptoms.
- Healthy Diet: Eating a balanced diet low in saturated fats and cholesterol can help manage underlying conditions like high blood pressure and diabetes.
- Weight Management: Losing excess weight reduces strain on the circulatory system.
Medications
In addition to lifestyle changes, medications may be prescribed to manage symptoms and reduce the risk of complications.
- Cholesterol-Lowering Drugs: These medications reduce plaque buildup in the arteries.
- Blood Pressure Medications: Controlling blood pressure helps protect the arteries.
- Diabetes Medications: Managing blood sugar levels is essential for those with diabetes.
- Antiplatelet Drugs: These medications prevent blood clots from forming.
Surgical Procedures
In severe cases, surgical interventions may be necessary to restore blood flow to the legs.
- Angioplasty: A procedure to widen narrowed arteries using a balloon catheter.
- Stent Placement: A small mesh tube is inserted to keep the artery open.
- Bypass Surgery: A surgical procedure to create a new path for blood flow around the blocked artery.
- Atherectomy: A procedure to remove plaque from the arteries.
Preventing Complications
Preventing complications is a key aspect of managing this condition. By taking proactive steps, individuals can reduce the risk of serious outcomes such as infections, ulcers, or amputations.
Foot Care
Proper foot care is essential for individuals with this condition. Poor circulation increases the risk of foot problems, including infections and ulcers.
- Daily Inspection: Check your feet daily for cuts, sores, or redness.
- Proper Footwear: Wear comfortable shoes that fit well and protect your feet.
- Moisturize: Keep your feet moisturized to prevent dry, cracked skin.
- Professional Care: Visit a podiatrist regularly for professional foot care.
Monitoring Underlying Conditions
Managing conditions such as diabetes, high blood pressure, and high cholesterol is crucial for preventing complications. Regular monitoring and adherence to treatment plans can significantly reduce the risk of further artery damage.
Living with the Condition
Living with this circulatory condition requires ongoing management and commitment to a healthy lifestyle. While it may present challenges, many individuals can lead active and fulfilling lives with proper care.
Emotional and Mental Health
Dealing with chronic conditions can take a toll on mental health. It is important to seek support from healthcare providers, family, and friends. Joining support groups or counseling sessions can also help individuals cope with the emotional aspects of living with this condition.
Staying Active
Staying physically active is vital for maintaining mobility and improving circulation. Low-impact exercises such as walking, swimming, or cycling can be beneficial. Always consult a healthcare provider before starting any new exercise program.
Education and Awareness
Educating yourself about the condition and staying informed about new treatments and research can empower you to make better decisions about your health. Attending workshops or seminars and reading reliable sources of information can enhance your understanding of the disease.