Perioral dermatitis, often abbreviated as PD, is a common skin condition that primarily affects the area around the mouth. It manifests as a persistent rash characterized by redness, small bumps, and sometimes scaling. While it may look similar to acne or eczema, perioral dermatitis has distinct causes and treatment approaches. Understanding this condition can help individuals identify it early and seek appropriate care to prevent complications.
What Is Perioral Dermatitis?
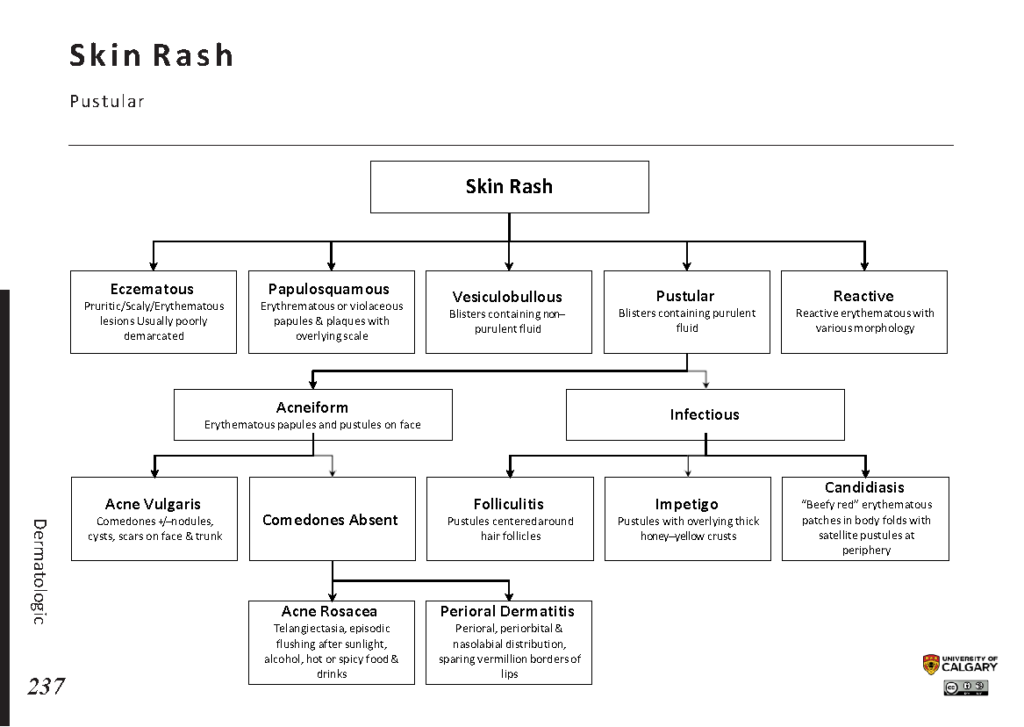
Perioral dermatitis is a type of inflammatory skin condition that occurs around the mouth. In some cases, it can also spread to the areas around the nose and eyes. The rash typically consists of clusters of small, red bumps or pustules, which may be accompanied by mild peeling or flakiness. Unlike acne, these bumps do not contain blackheads or whiteheads, and they often cause a burning or stinging sensation rather than itching.
This condition is more common in women, particularly those between the ages of 16 and 45, though it can occur in men and children as well. Despite its prevalence, many people remain unaware of what causes it and how to manage it effectively.
Causes of Perioral Dermatitis
The exact cause of perioral dermatitis remains unclear, but several factors are believed to contribute to its development. These include:
Topical Steroid Use
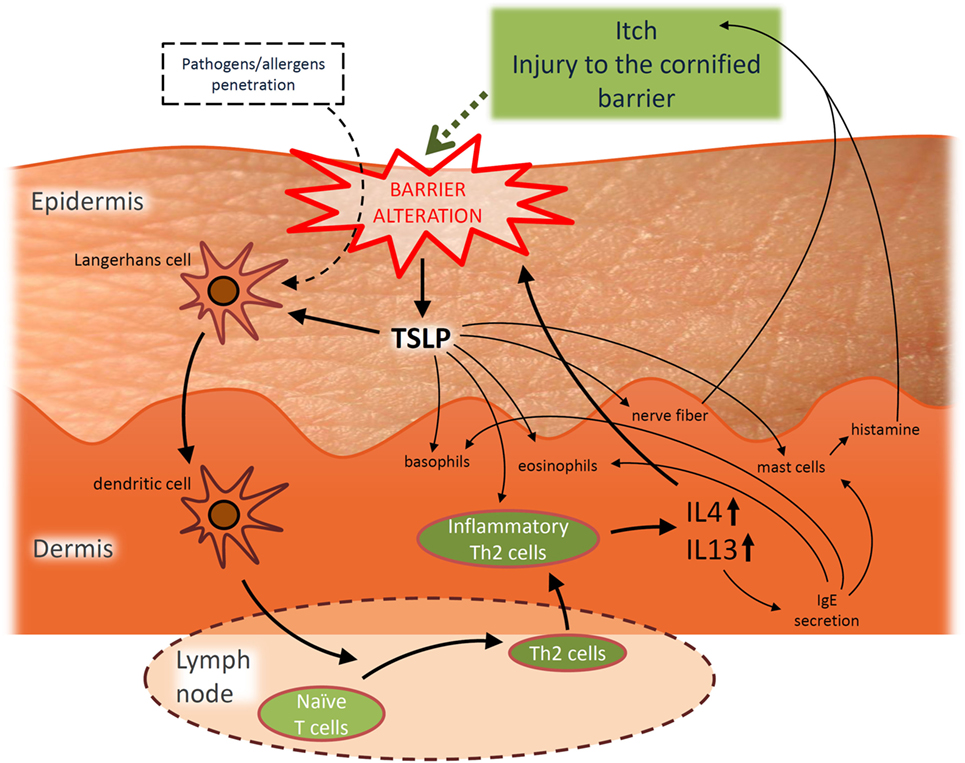
- Prolonged use of topical corticosteroids, especially on the face, is one of the leading triggers of perioral dermatitis. These medications, often prescribed for conditions like eczema or allergic reactions, can disrupt the skin’s natural barrier and lead to irritation when overused.
- Inhaled steroids, such as those used for asthma, may also increase the risk of developing this condition.
Cosmetic Products
- Heavy or occlusive skincare products, including moisturizers, foundations, and sunscreens, can clog pores and irritate sensitive facial skin.
- Fragrances and other chemical additives in cosmetics may exacerbate inflammation, particularly in individuals with sensitive skin.
Fluoridated Toothpaste
- Some studies suggest a potential link between fluoride-containing toothpaste and perioral dermatitis. Fluoride may irritate the delicate skin around the mouth, especially if it comes into frequent contact during brushing.
Hormonal Changes
- Hormonal fluctuations, such as those occurring during pregnancy, menstruation, or menopause, can make the skin more susceptible to irritation and inflammation.
Environmental Factors
- Exposure to harsh weather conditions, pollution, or excessive sunlight can weaken the skin’s protective barrier, making it more prone to developing rashes.
Bacterial Involvement
- While not fully understood, certain bacteria present on the skin may play a role in triggering or worsening perioral dermatitis.
Symptoms of Perioral Dermatitis
Recognizing the symptoms of perioral dermatitis is crucial for timely diagnosis and treatment. Common signs include:
Redness and Inflammation
- A noticeable reddening of the skin around the mouth is one of the earliest indicators of this condition.
- The affected area may feel warm to the touch due to increased blood flow caused by inflammation.
Small Bumps or Pustules
- Tiny red or flesh-colored bumps often appear in clusters around the mouth. These bumps may resemble pimples but lack the typical characteristics of acne lesions.
- In some cases, the bumps may contain pus, giving them a yellowish appearance.
Dryness and Scaling
- The skin around the mouth may become dry and flaky, leading to discomfort and tightness.
- This dryness can worsen if the individual attempts to scrub or exfoliate the area aggressively.
Burning or Stinging Sensation
- Unlike other rashes that tend to itch, perioral dermatitis often causes a burning or stinging sensation, particularly after applying skincare products or eating spicy foods.
Sparing of the Vermilion Border
- An interesting feature of this condition is that the rash typically spares the vermilion border, which is the line where the lips meet the surrounding skin. This creates a clear demarcation between the affected and unaffected areas.
Treatment Options for Perioral Dermatitis
Treating perioral dermatitis requires patience and consistency, as the condition can take weeks or even months to resolve completely. The following treatment strategies are commonly recommended:
Discontinuing Triggering Products
- The first step in managing perioral dermatitis is identifying and eliminating any potential triggers. This includes discontinuing the use of topical steroids, switching to gentle skincare products, and avoiding fluoridated toothpaste.
- It is important to note that stopping steroid creams abruptly can sometimes worsen symptoms temporarily. A healthcare provider may recommend tapering off these medications gradually under medical supervision.
Topical Antibiotics
- For mild to moderate cases, doctors often prescribe non-steroidal topical antibiotics, such as metronidazole gel or erythromycin ointment. These medications help reduce bacterial involvement and calm inflammation.
- Patients should apply these treatments sparingly and follow their healthcare provider’s instructions carefully to avoid further irritation.
Oral Antibiotics
- In more severe cases, oral antibiotics like tetracycline or doxycycline may be prescribed. These systemic medications target widespread inflammation and provide faster relief compared to topical treatments.
- Since long-term antibiotic use carries risks, such as antibiotic resistance, patients must adhere strictly to their prescribed regimen and attend follow-up appointments.
Gentle Skincare Routine
- Maintaining a simple and gentle skincare routine is essential for healing the skin. Opt for fragrance-free cleansers and moisturizers designed for sensitive skin.
- Avoid using scrubs, toners, or any product containing alcohol, retinoids, or alpha hydroxy acids until the rash has cleared.
Photoprotection
- Protecting the skin from ultraviolet radiation is critical, as sun exposure can exacerbate inflammation. Use a broad-spectrum sunscreen formulated for sensitive skin and wear hats or scarves for additional protection.
Lifestyle Modifications
- Adopting healthy lifestyle habits can support overall skin health. Stay hydrated, eat a balanced diet rich in antioxidants, and minimize stress through relaxation techniques like yoga or meditation.
When to See a Healthcare Provider
While perioral dermatitis is generally not harmful, seeking professional advice is advisable if:
- The rash persists despite home care measures.
- Symptoms worsen or spread to other parts of the face.
- There is significant discomfort or impact on quality of life.
A dermatologist can perform a thorough evaluation to rule out other conditions with similar presentations, such as rosacea or seborrheic dermatitis. They can also tailor a treatment plan based on the severity of the condition and individual needs.
Preventing Recurrence
Once perioral dermatitis has resolved, taking preventive measures can reduce the likelihood of recurrence:
- Continue using gentle skincare products and avoid reintroducing known irritants.
- Be cautious with new cosmetic products and patch-test them before full application.
- Monitor hormonal changes and consult a healthcare provider if necessary.