Perimenopause, often abbreviated as PM, marks a significant transition in a woman’s life. It is the period leading up to menopause when hormonal changes begin to occur, signaling the eventual end of reproductive years. Understanding this phase is crucial for women as it helps them navigate the physical, emotional, and psychological shifts that come with it. In this article, we will explore the symptoms, causes, and management strategies associated with perimenopause to provide clarity and support for those experiencing it.

What is Perimenopause?
Perimenopause refers to the transitional phase before menopause when the ovaries gradually produce less estrogen. This phase can last for several years and typically begins in a woman’s forties, though it may start earlier for some. Unlike menopause, which is defined as the point when a woman has not had a menstrual period for twelve consecutive months, perimenopause involves fluctuating hormone levels and irregular menstrual cycles. During this time, women may experience a wide range of symptoms due to these hormonal changes.
Key Characteristics of Perimenopause
- Hormonal fluctuations
- Irregular menstrual cycles
- Gradual decline in fertility
- Physical and emotional symptoms
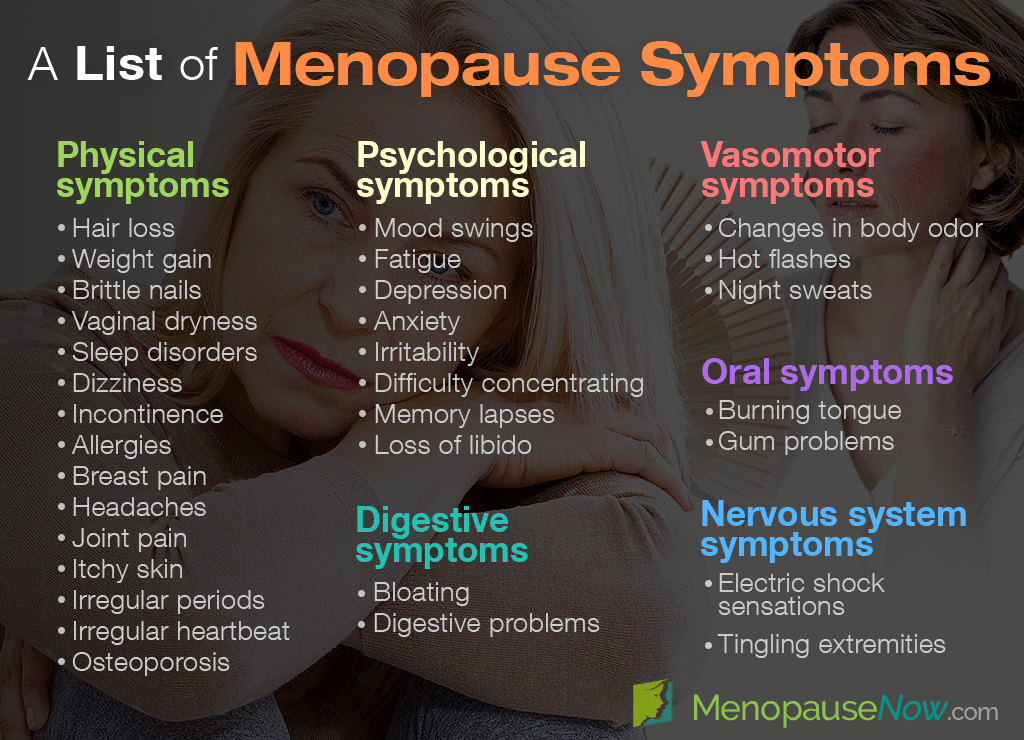
Symptoms of Perimenopause
The symptoms of perimenopause vary widely from person to person. Some women may experience mild discomfort, while others may find their symptoms significantly impact their daily lives. Below are some of the most common symptoms associated with this phase.
Menstrual Irregularities
One of the hallmark signs of perimenopause is changes in the menstrual cycle. Periods may become irregular, occurring more frequently or less frequently than usual. The flow may also vary, ranging from very light to unusually heavy. These changes are a result of fluctuating hormone levels, particularly estrogen and progesterone.
Hot Flashes and Night Sweats
Hot flashes are sudden feelings of warmth, often accompanied by sweating and a flushed face. They can occur at any time of the day but are particularly disruptive when they happen at night, leading to night sweats. These symptoms are caused by changes in the body’s thermoregulation due to declining estrogen levels.
Mood Changes
Hormonal fluctuations during perimenopause can also affect mood. Many women report increased irritability, anxiety, or feelings of sadness. These emotional changes can be challenging to manage, especially if they occur alongside other physical symptoms.
Sleep Disturbances
Difficulty falling asleep or staying asleep is another common symptom. Night sweats, anxiety, and hormonal imbalances can all contribute to disrupted sleep patterns. Poor sleep can further exacerbate other symptoms, such as fatigue and mood swings.
Vaginal and Bladder Changes
Decreased estrogen levels can lead to vaginal dryness, discomfort during intercourse, and an increased risk of urinary tract infections. These changes are often referred to as genitourinary syndrome and can significantly impact a woman’s quality of life.
Changes in Libido
Many women experience a decrease in sexual desire during perimenopause. This change can be attributed to hormonal fluctuations, physical discomfort, or emotional factors such as stress and fatigue.
Weight Gain and Metabolic Changes
It is common for women to notice changes in their body composition during perimenopause. Weight gain, particularly around the abdomen, can occur due to a slower metabolism. Hormonal changes may also increase the risk of conditions such as insulin resistance and high cholesterol.
Causes of Perimenopause
Perimenopause is primarily caused by the natural aging process and the gradual decline in ovarian function. As women age, their ovaries produce less estrogen and progesterone, two hormones that regulate the menstrual cycle and play a role in maintaining overall health. While the exact timing and progression of perimenopause vary, certain factors can influence its onset and severity.
Natural Aging Process
The most significant factor contributing to perimenopause is the natural decline in ovarian function. Over time, the number of eggs in the ovaries decreases, and the quality of the remaining eggs diminishes. This decline leads to irregular ovulation and fluctuating hormone levels.
Genetic Factors
Family history can play a role in determining when perimenopause begins. If a woman’s mother or sisters experienced early perimenopause, she may be more likely to do so as well. Genetic predisposition can influence both the timing and intensity of symptoms.
Lifestyle and Environmental Factors
Certain lifestyle choices and environmental exposures can impact the onset and severity of perimenopause. Smoking, excessive alcohol consumption, poor diet, and chronic stress may accelerate the decline in ovarian function. Additionally, exposure to environmental toxins and endocrine disruptors can interfere with hormonal balance.
Medical Interventions
In some cases, medical interventions such as surgery or treatments like chemotherapy can induce perimenopause. For example, the removal of the ovaries (oophorectomy) or radiation therapy can cause an abrupt drop in estrogen levels, leading to immediate onset of perimenopausal symptoms.
Management Strategies for Perimenopause
While perimenopause is a natural phase of life, there are several strategies women can adopt to manage its symptoms and maintain their overall well-being. These approaches include lifestyle modifications, medical treatments, and alternative therapies.
Lifestyle Modifications
Healthy lifestyle habits can significantly alleviate many symptoms of perimenopause. Below are some effective strategies:
- Dietary Changes: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help stabilize energy levels and support hormonal balance. Foods containing phytoestrogens, such as soy and flaxseeds, may also help mitigate symptoms.
- Regular Exercise: Physical activity can improve mood, reduce hot flashes, and promote better sleep. Activities such as walking, yoga, and strength training are particularly beneficial.
- Stress Management: Techniques such as meditation, deep breathing exercises, and mindfulness can help reduce stress and improve emotional well-being.
- Adequate Sleep: Establishing a consistent sleep routine and creating a restful environment can help combat sleep disturbances.
Hormone Replacement Therapy
Hormone replacement therapy involves taking medications containing estrogen and progesterone to replenish declining hormone levels. This treatment can effectively relieve symptoms such as hot flashes, night sweats, and vaginal dryness. However, it is essential to discuss the risks and benefits with a healthcare provider, as hormone therapy may not be suitable for everyone.
Non-Hormonal Medications
For women who cannot or prefer not to use hormone replacement therapy, non-hormonal medications may provide relief. Antidepressants, blood pressure medications, and certain seizure medications have been shown to reduce hot flashes and improve mood in some women.
Vaginal Treatments
To address vaginal dryness and discomfort, topical treatments such as moisturizers and lubricants can be highly effective. Low-dose vaginal estrogen therapy is another option that can restore moisture and elasticity without significantly affecting systemic hormone levels.
Alternative Therapies
Some women find relief through complementary and alternative therapies. These may include:
- Herbal Supplements: Black cohosh, red clover, and evening primrose oil are commonly used to alleviate symptoms, although scientific evidence supporting their efficacy is mixed.
- Acupuncture: This traditional Chinese medicine technique may help reduce hot flashes and improve sleep quality.
- Mind-Body Practices: Yoga, tai chi, and other mind-body practices can promote relaxation and enhance overall well-being.
Seeking Professional Guidance
Managing perimenopause effectively often requires personalized care. Women experiencing severe or disruptive symptoms should consult a healthcare provider for guidance. A doctor can perform tests to confirm the onset of perimenopause and rule out other potential causes of symptoms. They can also recommend appropriate treatments based on individual needs and medical history.
Regular check-ups during perimenopause are essential for monitoring bone health, cardiovascular health, and other aspects of well-being. Early intervention can help prevent long-term complications such as osteoporosis and heart disease, which may become more prevalent after menopause.
Emotional Support and Community
Perimenopause can be an emotionally challenging time, and seeking support from friends, family, or support groups can make a significant difference. Sharing experiences with others who are going through similar changes can provide comfort and practical advice. Online forums and local support groups offer valuable resources for women navigating this transition.
Conclusion
Perimenopause is a natural and inevitable phase of life, but it does not have to be overwhelming. By understanding its symptoms, causes, and management options, women can take proactive steps to maintain their health and well-being during this transformative period.