Pericarditis, often abbreviated as PC, is a medical condition characterized by inflammation of the pericardium, the protective sac-like membrane that surrounds the heart. This inflammation can lead to discomfort and complications if not properly managed. While it may sound alarming, understanding the causes, symptoms, diagnosis, and treatment options for this condition can help individuals navigate their health journey more effectively.
What is the Pericardium?
The pericardium is a double-layered structure that envelops the heart. It serves several essential functions, including:
- Providing a protective barrier to shield the heart from external infections or injuries
- Reducing friction between the heart and surrounding tissues during heartbeats
- Maintaining the heart’s position within the chest cavity
When this delicate lining becomes inflamed, it can interfere with these functions, leading to pain and other symptoms associated with pericarditis.
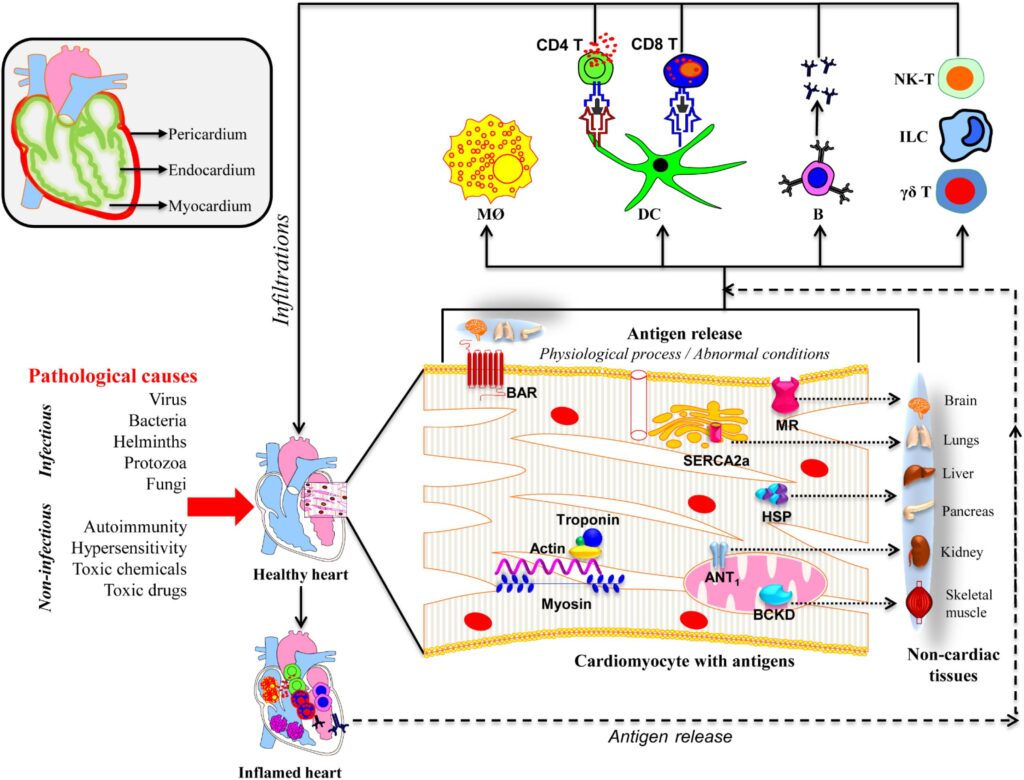
Causes of Pericarditis
There are numerous potential causes of pericarditis, ranging from infections to systemic diseases. Below are some of the most common factors that contribute to the development of this condition:
Infectious Causes
Infections caused by viruses, bacteria, fungi, or parasites are among the leading causes of pericarditis. Viral infections, in particular, are responsible for many cases. Common viral culprits include coxsackievirus, echovirus, and influenza virus. Bacterial infections, although less frequent, tend to cause more severe forms of pericarditis and require prompt treatment.
Autoimmune Disorders
Autoimmune conditions occur when the body’s immune system mistakenly attacks its own tissues. Diseases such as lupus, rheumatoid arthritis, and scleroderma can trigger inflammation of the pericardium. In these cases, managing the underlying autoimmune disorder is crucial for alleviating symptoms of pericarditis.
Trauma or Injury
Physical trauma to the chest, whether from an accident, surgery, or invasive medical procedures like cardiac catheterization, can damage the pericardium and lead to inflammation. Even minor injuries may sometimes result in pericarditis, especially if they affect the integrity of the pericardial layers.
Medications and Treatments
Certain medications have been linked to pericarditis as a rare side effect. These include drugs used in cancer treatment, such as chemotherapy agents, and some antibiotics. Additionally, radiation therapy targeting the chest area can irritate the pericardium and cause inflammation.
Other Contributing Factors
Other possible causes include kidney failure, which can lead to uremic pericarditis due to toxin buildup, and metabolic disorders. Idiopathic pericarditis, where no specific cause can be identified, is also relatively common and accounts for a significant proportion of cases.
Symptoms of Pericarditis
The symptoms of pericarditis vary depending on the severity and underlying cause but typically include:
- Chest pain, often sharp and stabbing, that worsens with deep breaths or lying down
- Fever and chills, particularly in cases caused by infections
- Shortness of breath, especially during physical activity
- A dry cough or hoarseness
- Fatigue and general weakness
One hallmark feature of pericarditis-related chest pain is its improvement when sitting up or leaning forward. This positional relief occurs because these postures reduce pressure on the inflamed pericardium.
Diagnosing Pericarditis
Accurate diagnosis is critical to ensure appropriate treatment. Healthcare providers rely on a combination of clinical evaluation, imaging studies, and laboratory tests to confirm pericarditis.
Medical History and Physical Examination
During the initial consultation, doctors will inquire about the patient’s symptoms, medical history, and any recent illnesses or injuries. A thorough physical examination may reveal signs such as abnormal heart sounds, known as a pericardial friction rub, which occurs due to the inflamed layers of the pericardium rubbing against each other.
Imaging Studies
Imaging plays a key role in diagnosing pericarditis. The following techniques are commonly employed:
- Echocardiogram: This ultrasound-based test provides detailed images of the heart and pericardium, helping detect fluid accumulation or thickening of the pericardial layers.
- Chest X-ray: Although less specific, a chest X-ray can show an enlarged cardiac silhouette if there is significant fluid buildup around the heart.
- Magnetic Resonance Imaging (MRI) or Computed Tomography (CT): These advanced imaging modalities offer high-resolution views of the pericardium and are useful for complex cases.
Laboratory Tests
Blood tests may be ordered to check for markers of inflammation, infection, or autoimmune activity. Elevated levels of C-reactive protein and white blood cells often indicate ongoing inflammation. Specific antibody tests might also be conducted if an autoimmune disorder is suspected.
Treatment Options for Pericarditis
Treatment aims to relieve symptoms, address the underlying cause, and prevent complications. The approach depends on the severity of the condition and its etiology.
Medications
Pharmacological interventions are the cornerstone of pericarditis management. Commonly prescribed medications include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These drugs, such as ibuprofen or aspirin, help reduce inflammation and alleviate pain.
- Colchicine: Often used alongside NSAIDs, colchicine has been shown to decrease the risk of recurrent episodes of pericarditis.
- Corticosteroids: In cases resistant to other treatments or associated with autoimmune conditions, corticosteroids like prednisone may be prescribed.
- Antibiotics or Antivirals: If an infectious agent is identified, targeted antimicrobial therapy is initiated.
Drainage Procedures
In situations where excessive fluid accumulates around the heart—a condition known as pericardial effusion—drainage may be necessary. Techniques include:
- Pericardiocentesis: A needle is inserted into the pericardial space to remove excess fluid.
- Pericardial Window: A surgical procedure creates an opening in the pericardium to allow continuous drainage.
Lifestyle Modifications
Patients are often advised to make certain lifestyle adjustments to support recovery. These recommendations may include:
- Avoiding strenuous activities until symptoms resolve
- Adopting a heart-healthy diet rich in fruits, vegetables, and whole grains
- Staying hydrated and getting adequate rest
Potential Complications of Pericarditis
If left untreated or inadequately managed, pericarditis can lead to serious complications. Some of the most notable risks include:
- Constrictive Pericarditis: Chronic inflammation can cause the pericardium to thicken and scar, restricting the heart’s ability to pump effectively.
- Cardiac Tamponade: Excessive fluid buildup compresses the heart, impairing its function and potentially becoming life-threatening.
- Recurrent Episodes: Without proper treatment, pericarditis may recur, leading to prolonged discomfort and increased healthcare needs.
Preventing Pericarditis
While not all cases of pericarditis can be prevented, certain measures can lower the risk of developing this condition:
- Treating underlying infections promptly to prevent their spread to the pericardium
- Managing chronic conditions like autoimmune disorders through regular follow-ups and adherence to prescribed therapies
- Avoiding unnecessary exposure to toxins or harmful substances that could irritate the pericardium
Vaccination against viral infections, maintaining good hygiene practices, and seeking timely medical care for chest injuries or symptoms can further reduce the likelihood of pericarditis.