Pericardial effusion, often abbreviated as PE, is a medical condition characterized by the abnormal accumulation of fluid in the pericardial space, which is the area between the layers of the sac-like structure surrounding the heart. This buildup of fluid can exert pressure on the heart, interfering with its ability to pump blood effectively. If left untreated, it can lead to serious complications, including cardiac tamponade, a life-threatening condition. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for this condition.
What Is Pericardial Effusion?
The pericardium is a double-layered membrane that surrounds the heart, providing protection and lubrication to allow the heart to beat efficiently. Normally, there is a small amount of fluid in the pericardial space to reduce friction as the heart contracts and relaxes. However, when excessive fluid accumulates in this space, it is referred to as pericardial effusion.
This condition can develop suddenly (acute) or over time (chronic). The severity of the condition depends on the volume of fluid, how quickly it accumulates, and whether it compresses the heart.
Causes of Pericardial Effusion
There are numerous potential causes of pericardial effusion, ranging from infections to systemic diseases. Below are some of the most common causes:
Infections
- Viral Infections: Viruses such as coxsackievirus and echovirus are common culprits. These infections often lead to inflammation of the pericardium, known as pericarditis, which can result in fluid accumulation.
- Bacterial Infections: Bacterial infections, including tuberculosis, can cause pericardial effusion. Tuberculosis-related pericardial effusion is more prevalent in regions where tuberculosis is endemic.
- Fungal Infections: Fungal infections are rare but can occur in individuals with weakened immune systems.
Inflammatory Conditions
- Autoimmune Disorders: Conditions such as lupus, rheumatoid arthritis, and scleroderma can trigger inflammation of the pericardium, leading to fluid buildup.
- Post-Cardiac Injury Syndrome: Also known as Dressler’s syndrome, this condition occurs after a heart attack or heart surgery and involves inflammation of the pericardium.
Cancer
- Malignant Tumors: Cancer that spreads to the pericardium, such as lung cancer, breast cancer, or lymphoma, can cause pericardial effusion.
- Radiation Therapy: Individuals who undergo radiation therapy for cancers near the chest may develop pericardial effusion as a side effect.
Kidney and Liver Diseases
- Chronic Kidney Disease: Impaired kidney function can lead to an imbalance of fluids and electrolytes, contributing to fluid accumulation in the pericardium.
- Liver Cirrhosis: Liver dysfunction can result in low protein levels in the blood, causing fluid to leak into the pericardial space.
Trauma and Medical Procedures
- Chest Trauma: Injuries to the chest, such as those sustained in car accidents, can damage the pericardium and lead to fluid accumulation.
- Invasive Procedures: Certain medical procedures, such as cardiac catheterization or pacemaker implantation, may inadvertently cause pericardial effusion.
Other Causes
- Hypothyroidism: An underactive thyroid gland can slow down the body’s metabolism, leading to fluid retention, including in the pericardium.
- Medications: Some drugs, such as hydralazine and isoniazid, have been associated with pericardial effusion as a rare side effect.
Symptoms of Pericardial Effusion
The symptoms of pericardial effusion vary depending on the rate of fluid accumulation and the underlying cause. In cases where the fluid builds up slowly, individuals may experience mild or no symptoms initially. However, rapid accumulation can lead to severe symptoms and complications. Common signs and symptoms include:
Chest Pain
Chest pain is one of the hallmark symptoms of pericardial effusion. The pain is often sharp and worsens when lying down or taking deep breaths. It may improve when sitting up or leaning forward.
Shortness of Breath
As the fluid presses on the heart, it can impair the heart’s ability to fill with blood, leading to difficulty breathing. Shortness of breath may worsen with physical activity or when lying flat.
Palpitations
Some individuals may feel their heart racing or fluttering due to the strain placed on the heart by the excess fluid.
Fatigue
Reduced cardiac output caused by pericardial effusion can result in persistent fatigue and weakness.
Swelling
Fluid retention can cause swelling in the legs, ankles, or abdomen. This is particularly common in cases related to kidney or liver disease.
Low Blood Pressure
When the heart is compressed by the fluid, it may struggle to pump enough blood, leading to low blood pressure and dizziness.
Diagnosis of Pericardial Effusion
Diagnosing pericardial effusion involves a combination of clinical evaluation, imaging tests, and laboratory investigations. Early and accurate diagnosis is crucial to prevent complications.
Physical Examination
A healthcare provider may detect signs of pericardial effusion during a physical examination. These may include muffled heart sounds, distended neck veins, and low blood pressure.
Imaging Tests
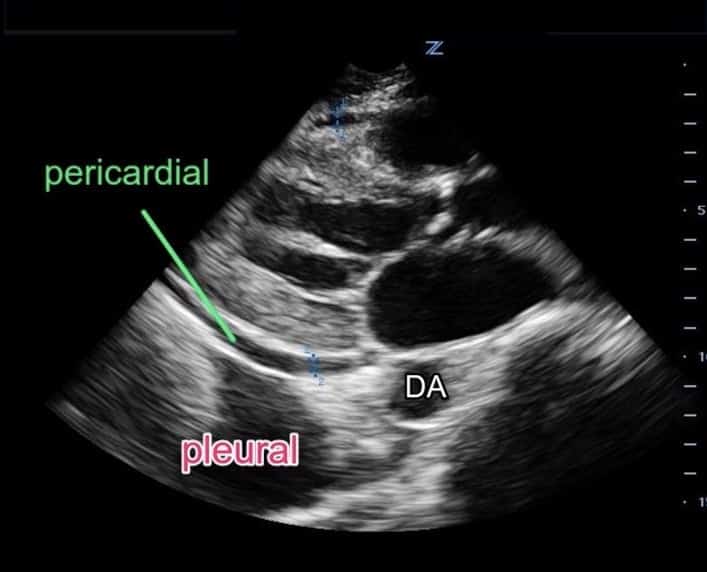
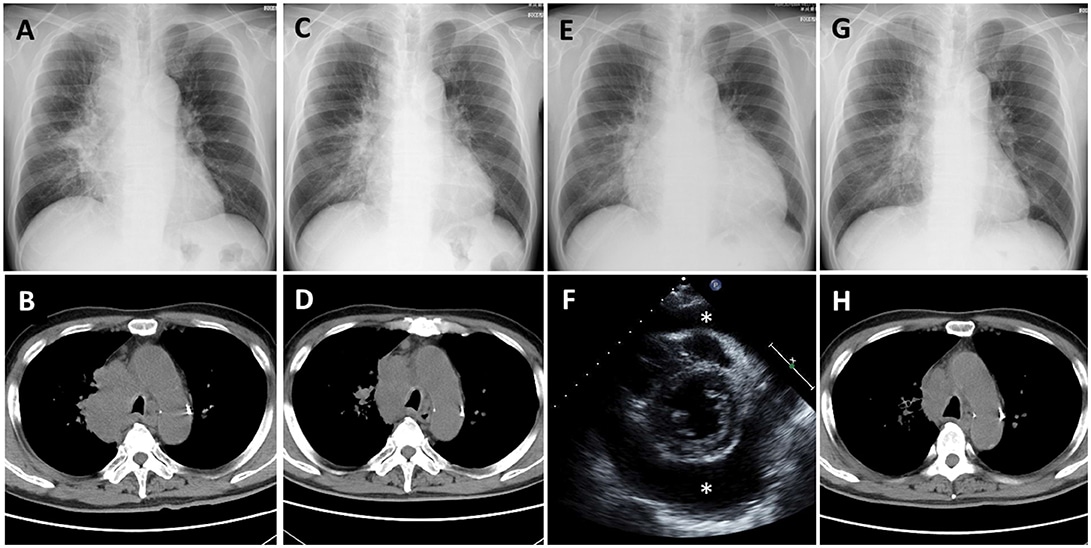
- Echocardiogram: This ultrasound of the heart is the primary tool used to diagnose pericardial effusion. It allows doctors to visualize the pericardium and assess the amount and impact of fluid accumulation.
- Chest X-Ray: A chest X-ray may reveal an enlarged heart silhouette, which can indicate the presence of pericardial effusion.
- Computed Tomography (CT) Scan: A CT scan provides detailed images of the heart and surrounding structures, helping to identify the cause of the effusion.
- Magnetic Resonance Imaging (MRI): MRI is another imaging modality that can provide precise information about the pericardium and the nature of the fluid.
Laboratory Tests
- Blood Tests: Blood tests can help identify underlying conditions, such as infections, autoimmune disorders, or kidney and liver dysfunction.
- Pericardiocentesis: In some cases, a sample of the pericardial fluid may be removed using a needle and analyzed to determine its composition and possible cause.
Treatment Options for Pericardial Effusion
The treatment of pericardial effusion depends on the underlying cause, the severity of symptoms, and the risk of complications. The goal of treatment is to relieve symptoms, address the root cause, and prevent recurrence.
Observation
In cases where the effusion is small and not causing symptoms, close monitoring may be sufficient. Regular follow-up appointments and imaging tests are essential to ensure the condition does not worsen.
Medications
- Anti-Inflammatory Drugs: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to reduce inflammation and alleviate symptoms.
- Antibiotics: If the effusion is caused by a bacterial infection, antibiotics are necessary to treat the infection.
- Diuretics: These medications help reduce fluid retention and may be used in cases related to heart failure or kidney disease.
Procedures
- Pericardiocentesis: This procedure involves inserting a needle into the pericardial space to drain the excess fluid. It provides immediate relief and can also help diagnose the cause of the effusion.
- Pericardial Window: In recurrent or chronic cases, a surgical procedure called a pericardial window may be performed. This involves creating an opening in the pericardium to allow fluid to drain into the chest cavity.
- Pericardiectomy: In severe or persistent cases, part or all of the pericardium may need to be surgically removed.
Treatment of Underlying Conditions
Addressing the underlying cause of pericardial effusion is critical for long-term management. For example:
- Treating infections with appropriate medications.
- Managing autoimmune disorders with immunosuppressive therapies.
- Optimizing treatment for chronic conditions like kidney disease or hypothyroidism.
Lifestyle Modifications
In addition to medical treatments, certain lifestyle changes can support recovery and reduce the risk of recurrence:
- Adopting a heart-healthy diet low in sodium.
- Exercising regularly, as tolerated.
- Avoiding alcohol and smoking.