Pemphigus Vulgaris, often abbreviated as PV, is a rare autoimmune disorder that affects the skin and mucous membranes. This condition leads to the formation of painful blisters and sores, significantly impacting the quality of life for those affected. In this article, we will explore the causes, symptoms, and available treatments for this challenging disease.
Understanding Pemphigus Vulgaris
Pemphigus Vulgaris is part of a group of blistering diseases that primarily affect the skin and mucosal surfaces. It is considered an autoimmune disorder, meaning that the immune system mistakenly attacks healthy cells in the body. Specifically, this condition targets proteins that hold skin cells together, leading to the breakdown of these connections and the formation of blisters.
How Does Pemphigus Vulgaris Develop?
The development of this condition begins when the immune system produces antibodies against desmogleins, which are proteins responsible for binding skin cells together. These proteins are found in desmosomes, structures that act like glue to keep skin cells attached. When the immune system attacks these proteins, the bonds between skin cells weaken, causing the layers of the skin to separate and form blisters.
Who Is at Risk?
- Genetic predisposition: Some individuals may have a genetic susceptibility to developing this condition.
- Age and gender: It most commonly affects people between the ages of forty and sixty, and certain studies suggest it may be more prevalent in men than women.
- Ethnicity: People of Jewish descent, particularly those of Ashkenazi heritage, appear to have a higher risk of developing the condition.
Symptoms of Pemphigus Vulgaris
The symptoms of this condition can vary from person to person, but they typically involve the formation of blisters and sores on the skin and mucous membranes. These symptoms can be both physically and emotionally distressing due to their appearance and the discomfort they cause.
Common Signs and Symptoms
- Blisters on the skin: These blisters are fragile and can rupture easily, leaving behind painful sores. They often appear on the scalp, face, chest, and back.
- Mouth sores: One of the earliest signs of the condition is the presence of painful sores in the mouth. These sores can make eating and drinking difficult.
- Blisters in mucous membranes: In addition to the mouth, blisters may also develop in other mucous membranes, such as the throat, nose, eyes, and genitals.
- Skin peeling: The outer layer of the skin may peel off easily, even with minor friction or pressure.
Progression of Symptoms
In many cases, the condition begins with mild symptoms, such as small blisters or sores in the mouth. Over time, these symptoms can worsen and spread to other parts of the body. If left untreated, the blisters and sores can become infected, leading to further complications.
Causes of Pemphigus Vulgaris
While the exact cause of this condition remains unclear, researchers believe that a combination of genetic and environmental factors may contribute to its development. Understanding these potential triggers can help in managing and preventing flare-ups.
Autoimmune Mechanism
At its core, this condition is driven by an abnormal immune response. Normally, the immune system protects the body from harmful invaders like bacteria and viruses. However, in individuals with this condition, the immune system mistakenly targets desmogleins, disrupting the integrity of the skin and mucous membranes.
Potential Triggers
- Medications: Certain drugs, such as blood pressure medications or antibiotics, have been linked to triggering this condition in some individuals.
- Infections: Viral or bacterial infections may act as triggers for the onset of symptoms in genetically predisposed individuals.
- Environmental factors: Exposure to ultraviolet light, chemicals, or physical trauma may exacerbate the condition or trigger flare-ups.
Role of Genetics
Research suggests that genetics play a significant role in the development of this condition. Specific genes related to the immune system may increase the likelihood of developing an autoimmune response against desmogleins. Family history can sometimes provide clues about an individual’s risk.
Diagnosis of Pemphigus Vulgaris
Diagnosing this condition can be challenging due to its rarity and the similarity of its symptoms to other blistering disorders. A thorough evaluation by a healthcare professional is essential to confirm the diagnosis and rule out other conditions.
Clinical Examination
A dermatologist or healthcare provider will begin by examining the blisters and sores on the skin and mucous membranes. They may gently rub the skin near a blister to see if the top layer peels off easily, a test known as the Nikolsky sign. A positive result can indicate the presence of this condition.
Laboratory Tests
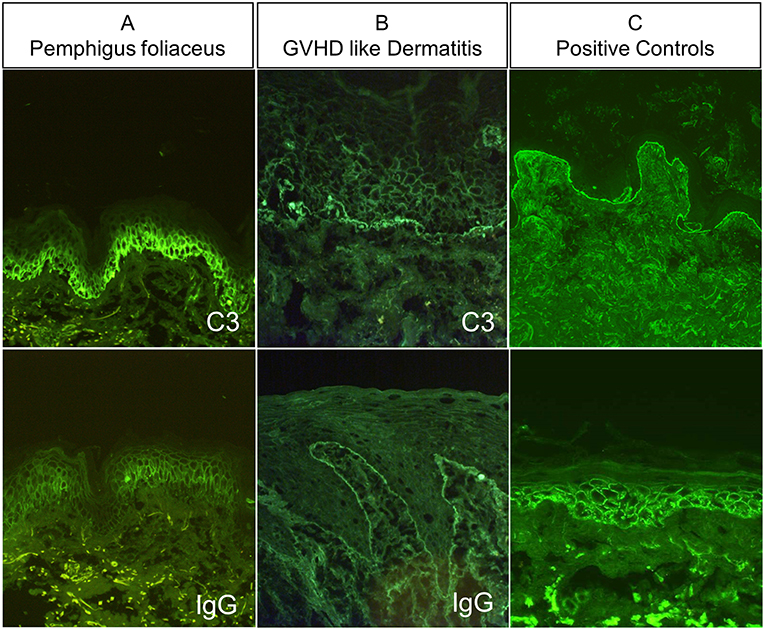
- Biopsy: A small sample of skin tissue may be taken and examined under a microscope to look for characteristic changes in the skin layers.
- Direct immunofluorescence: This test involves taking a biopsy of the skin and using special dyes to detect antibodies targeting desmogleins.
- Blood tests: Blood samples may be analyzed to check for the presence of specific antibodies associated with this condition.
Treatment Options for Pemphigus Vulgaris
While there is no cure for this condition, various treatments are available to manage symptoms and prevent complications. The primary goal of treatment is to reduce blister formation, promote healing, and minimize the risk of infection.
Medications
- Corticosteroids: These anti-inflammatory drugs are often the first line of treatment. They work by suppressing the immune system to reduce the production of harmful antibodies.
- Immunosuppressants: Medications such as azathioprine or mycophenolate mofetil may be prescribed to further suppress the immune system and reduce reliance on corticosteroids.
- Rituximab: This medication targets specific immune cells involved in the autoimmune response and has shown promise in treating severe cases.
Topical Treatments
For localized symptoms, topical treatments such as corticosteroid creams or ointments may be applied directly to the affected areas. These can help reduce inflammation and promote healing of the skin.
Lifestyle and Home Remedies
In addition to medical treatments, certain lifestyle adjustments can help manage symptoms and improve overall well-being.
- Oral care: Maintaining good oral hygiene is crucial, especially for individuals with mouth sores. Using a soft toothbrush and avoiding spicy or acidic foods can help minimize irritation.
- Protecting the skin: Wearing loose-fitting clothing and avoiding activities that cause friction or trauma to the skin can help prevent new blisters from forming.
- Dietary considerations: A balanced diet rich in vitamins and minerals can support the immune system and aid in the healing process.
Monitoring and Follow-Up
Regular follow-up appointments with a healthcare provider are essential to monitor the effectiveness of treatment and make any necessary adjustments. Blood tests may be performed periodically to check for side effects of medications and ensure that the condition is being adequately managed.
Complications Associated with Pemphigus Vulgaris
If left untreated or poorly managed, this condition can lead to several complications that may require additional medical attention.
Infections
The open sores and blisters caused by this condition create an entry point for bacteria, increasing the risk of infections. These infections can spread to deeper layers of the skin or even enter the bloodstream, leading to more serious health issues.
Nutritional Deficiencies
Painful mouth sores can make eating and drinking difficult, potentially leading to malnutrition or dehydration. Working with a nutritionist to develop a suitable diet plan can help address these concerns.
Psychological Impact
The visible nature of the blisters and sores can take a toll on an individual’s mental health, leading to feelings of embarrassment, anxiety, or depression. Seeking support from mental health professionals or joining a support group can be beneficial.
Emerging Research and Future Directions
Ongoing research into the causes and treatments of this condition holds promise for improved outcomes in the future. Scientists are exploring new therapies, including biologic agents and gene therapy, that may offer more targeted and effective solutions.
Advances in Treatment
Recent advancements in understanding the immune system’s role in this condition have paved the way for innovative treatments. For example, biologic therapies that specifically target immune cells involved in the disease process are being studied in clinical trials.
Focus on Early Detection
Efforts are also underway to improve early detection and diagnosis. Developing more accurate diagnostic tools and raising awareness among healthcare providers can help ensure timely intervention and better management of symptoms.