Pelvic Inflammatory Disease, commonly referred to as PID, is a serious infection that affects the female reproductive organs. It can lead to severe complications if left untreated, including infertility, chronic pelvic pain, and ectopic pregnancy. This article provides an in-depth exploration of the causes, symptoms, diagnosis, and treatment options for this condition.
Understanding Pelvic Inflammatory Disease
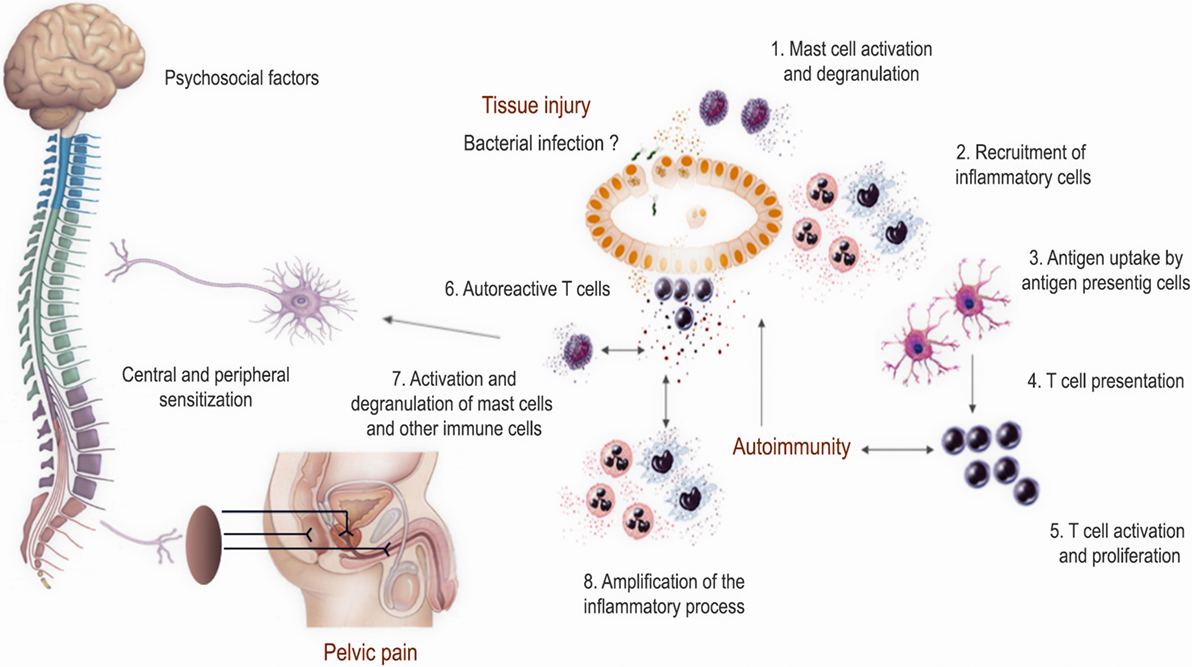
Pelvic Inflammatory Disease primarily involves the infection and inflammation of the upper genital tract in women. The infection often starts in the vagina or cervix and spreads upward to affect the uterus, fallopian tubes, and ovaries. While it is most commonly caused by sexually transmitted infections, other factors can also contribute to its development.
Causes of Pelvic Inflammatory Disease
The primary cause of Pelvic Inflammatory Disease is bacteria entering the reproductive tract. Below are the main sources of these bacterial infections:
- Sexually Transmitted Infections: Bacteria such as Chlamydia trachomatis and Neisseria gonorrhoeae are responsible for many cases of this disease. These bacteria are typically transmitted through unprotected sexual intercourse.
- Vaginal Flora Imbalance: Sometimes, the natural bacteria present in the vagina can overgrow and travel to the upper reproductive organs, leading to infection.
- Medical Procedures: Certain procedures, such as the insertion of an intrauterine device, endometrial biopsy, or dilation and curettage, can introduce bacteria into the reproductive tract.
- Childbirth or Miscarriage: After childbirth or miscarriage, the cervix may remain slightly open, allowing bacteria to ascend into the reproductive organs.
Risk Factors for Developing Pelvic Inflammatory Disease
While anyone with female reproductive organs can develop this condition, certain factors increase the likelihood of infection:
- Engaging in unprotected sexual activity
- Having multiple sexual partners
- A history of sexually transmitted infections
- Being under the age of 25
- Douching, which disrupts the natural balance of vaginal bacteria
Symptoms of Pelvic Inflammatory Disease
The symptoms of this condition can vary widely, ranging from mild discomfort to severe pain. Some individuals may not experience any noticeable symptoms at all, making early detection challenging. Common signs include:
- Persistent pain in the lower abdomen or pelvis
- Abnormal vaginal discharge with a foul odor
- Irregular menstrual bleeding or spotting between periods
- Pain during sexual intercourse
- Painful urination
- Fever and chills
- Nausea and vomiting
In some cases, the symptoms may be mistaken for other conditions, such as appendicitis or ovarian cysts. Therefore, it is crucial to seek medical attention if any of these symptoms arise.
Diagnosing Pelvic Inflammatory Disease
Diagnosing this condition requires a combination of clinical evaluation, laboratory tests, and imaging studies. Healthcare providers use the following methods to confirm the presence of infection:
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. During the pelvic exam, they may check for tenderness in the reproductive organs and look for signs of abnormal discharge or inflammation.
Laboratory Tests
To identify the specific bacteria causing the infection, healthcare providers may order the following tests:
- Cervical Cultures: A swab is taken from the cervix to test for sexually transmitted infections like chlamydia and gonorrhea.
- Blood Tests: Blood samples may be analyzed to detect elevated white blood cell counts, which indicate infection.
- Urine Tests: These can help rule out urinary tract infections and identify sexually transmitted infections.
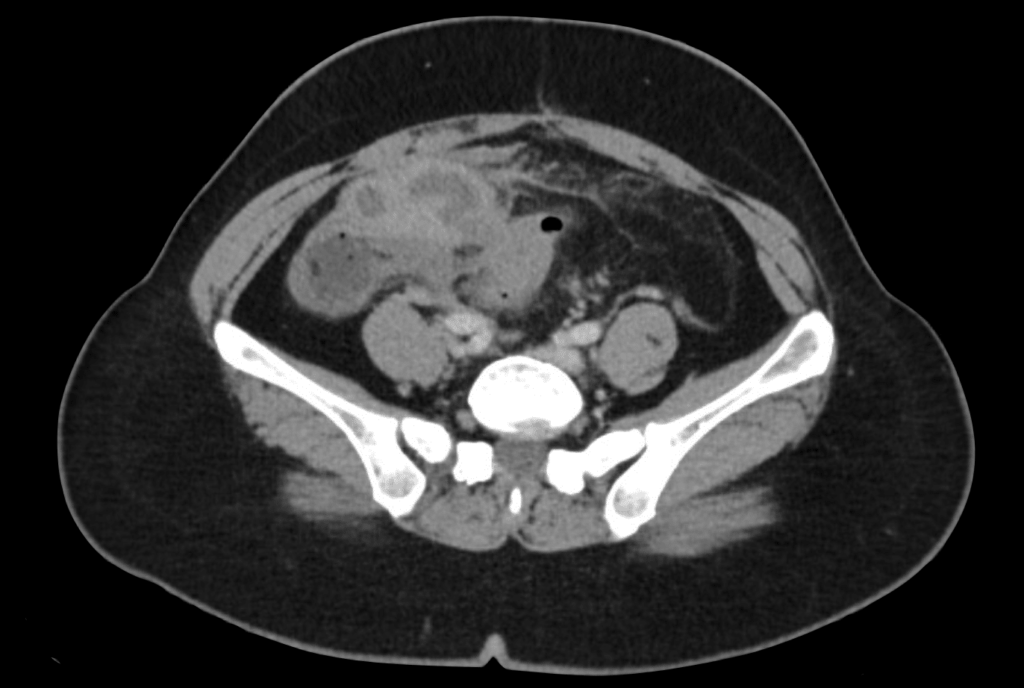
Imaging Studies
In some cases, imaging techniques such as ultrasound or magnetic resonance imaging may be used to visualize the reproductive organs and assess the extent of inflammation or damage.
Treatment Options for Pelvic Inflammatory Disease
Early and effective treatment is essential to prevent complications. The primary goal of treatment is to eliminate the infection, relieve symptoms, and preserve fertility. Below are the main approaches to managing this condition:
Antibiotic Therapy
Antibiotics are the cornerstone of treatment for this condition. Depending on the severity of the infection, antibiotics may be administered orally or intravenously. Commonly prescribed antibiotics include:
- Ceftriaxone
- Doxycycline
- Metronidazole
In severe cases, hospitalization may be necessary to administer intravenous antibiotics and closely monitor the patient’s response to treatment.
Pain Management
To alleviate pain and discomfort, healthcare providers may recommend over-the-counter pain relievers such as ibuprofen or acetaminophen. In some cases, stronger prescription medications may be required.
Treatment of Sexual Partners
To prevent reinfection, it is crucial for sexual partners to undergo testing and treatment for sexually transmitted infections. Abstaining from sexual activity until both partners have completed treatment is strongly advised.
Surgical Intervention
In rare cases where abscesses form in the reproductive organs, surgical intervention may be necessary. Procedures such as laparoscopy or drainage of abscesses can help remove infected tissue and prevent further complications.
Preventing Pelvic Inflammatory Disease
Prevention plays a vital role in reducing the risk of developing this condition. Below are some strategies to minimize the likelihood of infection:
- Practicing safe sex by using condoms consistently and correctly
- Undergoing regular screenings for sexually transmitted infections
- Avoiding douching, which can disrupt the natural balance of vaginal bacteria
- Seeking prompt treatment for any symptoms of infection
Vaccination
Vaccines are available to protect against certain sexually transmitted infections, such as human papillomavirus, which can indirectly reduce the risk of developing this condition.
Education and Awareness
Raising awareness about the risks and symptoms of this condition can empower individuals to seek timely medical care. Educational programs targeting young women and high-risk populations are particularly important.
Complications of Untreated Pelvic Inflammatory Disease
If left untreated, this condition can lead to several long-term complications, including:
- Infertility due to scarring of the fallopian tubes
- Ectopic pregnancy, where a fertilized egg implants outside the uterus
- Chronic pelvic pain that persists even after the infection has been treated
- Increased risk of recurrent infections
These complications underscore the importance of early diagnosis and treatment to preserve reproductive health.
Living with Pelvic Inflammatory Disease
Managing this condition requires a comprehensive approach that includes medical treatment, lifestyle modifications, and emotional support. Individuals diagnosed with this condition should work closely with their healthcare providers to develop a personalized care plan. Regular follow-up appointments are essential to monitor recovery and address any lingering symptoms.
Support groups and counseling can also provide valuable resources for individuals coping with the emotional and psychological impact of this condition. Connecting with others who have had similar experiences can foster a sense of community and resilience.