Patent Ductus Arteriosus, commonly abbreviated as PDA, is a congenital heart condition that affects the normal flow of blood in newborns. It occurs when a specific blood vessel, known as the ductus arteriosus, fails to close after birth. This small but critical passageway plays an essential role during fetal development by allowing blood to bypass the lungs until the baby begins breathing independently. However, if it remains open after birth, it can lead to complications. In this article, we will explore the condition in detail, covering its causes, symptoms, and available treatment options.
Understanding the Condition
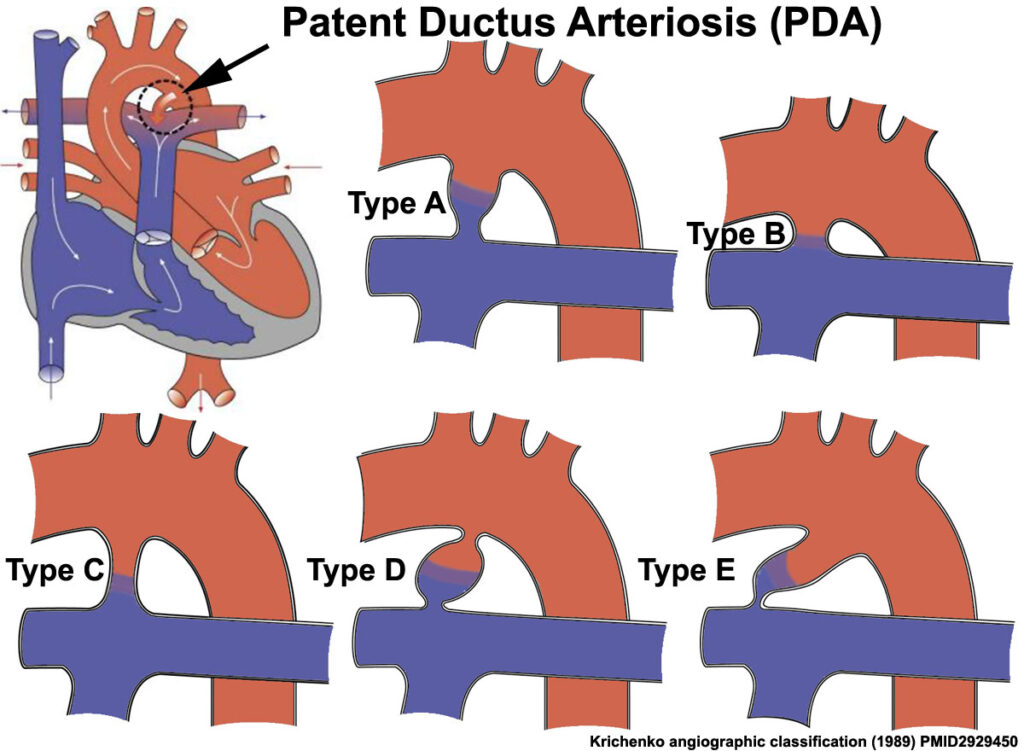
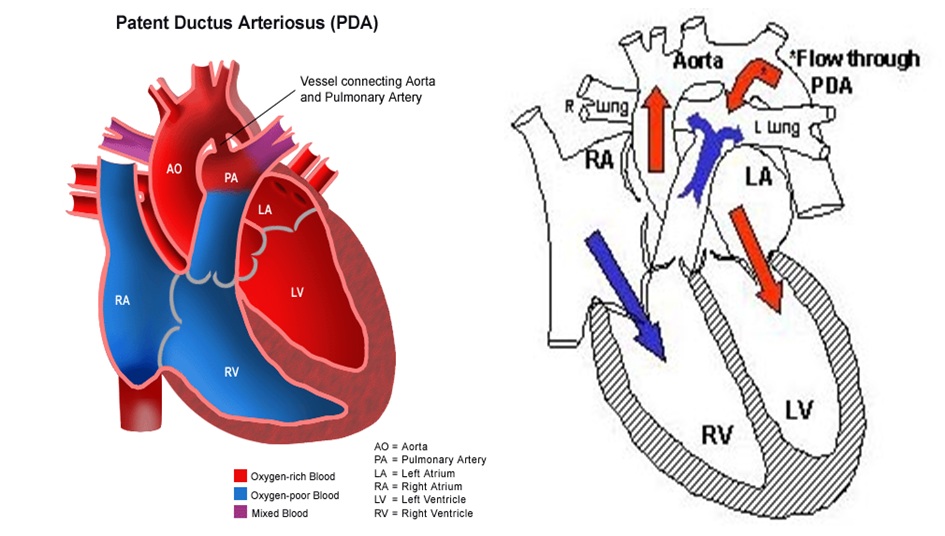
The ductus arteriosus is a temporary blood vessel present in all developing babies. During pregnancy, it connects two major arteries—the pulmonary artery and the aorta—allowing blood to flow directly from the heart to the body without passing through the lungs. This mechanism is crucial because the fetus receives oxygen from the mother’s bloodstream via the placenta, not the lungs.
After birth, the baby takes its first breath, and the lungs begin functioning. At this point, the ductus arteriosus is no longer needed and typically closes within the first few days or weeks of life. When it does not close as expected, the condition is referred to as Patent Ductus Arteriosus. This persistent opening allows oxygen-rich blood from the aorta to mix with oxygen-poor blood in the pulmonary artery, leading to an inefficient circulation process.
How Common Is This Condition?
- It is more frequently observed in premature infants compared to full-term babies.
- Approximately one in 2,000 full-term infants is affected.
- In premature babies, the incidence can be as high as 60% depending on their gestational age and weight at birth.
Causes of Patent Ductus Arteriosus
The exact cause of this condition is not always clear, but several factors may contribute to its development:
Genetic Factors
In some cases, genetic abnormalities or inherited conditions may increase the likelihood of the ductus arteriosus failing to close. For instance, certain syndromes such as Down syndrome are associated with a higher risk of congenital heart defects, including this condition.
Premature Birth
Premature infants are at a significantly higher risk due to underdeveloped organs and systems. The muscles surrounding the ductus arteriosus might not be strong enough to constrict and seal the vessel properly after birth.
Maternal Health and Environmental Factors
Certain maternal health conditions and environmental influences during pregnancy can also play a role:
- Rubella infection: If a mother contracts rubella (German measles) during pregnancy, it can interfere with the proper formation of the baby’s heart structures.
- Exposure to drugs or alcohol: Substance abuse during pregnancy has been linked to various congenital anomalies, including issues with the cardiovascular system.
- Lack of essential nutrients: Poor maternal nutrition, particularly deficiencies in folic acid, can increase the risk of heart defects in the developing fetus.
Symptoms of Patent Ductus Arteriosus
The symptoms of this condition vary depending on the size of the opening and the age of the child. In mild cases, there may be no noticeable signs, while larger openings can lead to significant health concerns.
Symptoms in Infants
For newborns and young children, common symptoms include:
- Rapid breathing: Babies may exhibit unusually fast or labored breathing, even when resting.
- Poor feeding: Difficulty feeding or taking less milk than usual can indicate underlying heart problems.
- Fatigue: Infants may appear excessively tired or lethargic.
- Sweating during feeds: Excessive sweating, especially while eating, is often a red flag.
- Poor growth: Failure to gain weight or grow at a normal rate despite adequate nutrition.
Symptoms in Older Children and Adults
If left untreated, this condition can persist into adulthood, leading to additional complications. Symptoms in older individuals may include:
- Shortness of breath: Particularly during physical activity or exercise.
- Heart palpitations: Irregular or rapid heartbeat sensations.
- Frequent respiratory infections: Recurring bouts of pneumonia or bronchitis.
- Tiredness: Persistent fatigue unrelated to exertion.
When to Seek Medical Attention
Parents should consult a pediatrician if they notice any of the above symptoms in their child. Early diagnosis and intervention are key to preventing long-term complications.
Diagnosis of Patent Ductus Arteriosus
A thorough evaluation by a healthcare provider is necessary to confirm the presence of this condition. Several diagnostic tools are used to identify and assess its severity:
Physical Examination
During a routine checkup, a doctor may detect a distinctive heart murmur using a stethoscope. This “machinery-like” sound is characteristic of blood flowing abnormally between the two connected arteries.
Imaging Tests
To confirm the diagnosis, imaging tests are conducted:
- Echocardiogram: An ultrasound of the heart provides detailed images of its structure and function, clearly showing the open ductus arteriosus.
- Chest X-ray: This test helps evaluate the size and shape of the heart and lungs, which may appear enlarged in severe cases.
- Electrocardiogram (ECG): Measures the electrical activity of the heart to detect irregularities in rhythm or structure.
Treatment Options for Patent Ductus Arteriosus
Treatment depends on the size of the opening, the patient’s age, and the presence of symptoms. In many cases, intervention is required to prevent complications such as heart failure or pulmonary hypertension.
Medications
For premature infants, medications like indomethacin or ibuprofen may be administered to help close the ductus arteriosus. These drugs work by constricting the blood vessel and promoting closure.
Catheter-Based Procedures
In older infants and children, minimally invasive techniques are often preferred:
- Catheterization: A thin tube called a catheter is inserted through a blood vessel in the groin and guided to the heart. A coil or plug is then placed inside the open ductus arteriosus to block blood flow.
Surgical Intervention
If medications and catheter-based methods are ineffective or unsuitable, surgery may be recommended. During the procedure, a surgeon ties off or clips the open vessel to stop abnormal blood flow.
Post-Treatment Care
Following treatment, regular follow-ups with a cardiologist are essential to monitor recovery and ensure the effectiveness of the intervention. Most patients experience significant improvement and go on to lead healthy lives.
Lifestyle Adjustments
While medical interventions address the immediate issue, certain lifestyle modifications can support overall cardiovascular health:
- Maintaining a balanced diet rich in fruits, vegetables, and whole grains.
- Engaging in regular physical activity appropriate for the individual’s age and condition.
- Avoiding exposure to secondhand smoke and other environmental pollutants.
Potential Complications
If left untreated, this condition can lead to serious complications over time. Some potential risks include:
- Heart failure: The extra workload on the heart can weaken its muscles and impair its ability to pump blood effectively.
- Pulmonary hypertension: Increased pressure in the lung arteries can damage the delicate tissues of the lungs.
- Infective endocarditis: Bacterial infections of the inner lining of the heart chambers and valves.
Preventing Long-Term Effects
Timely diagnosis and treatment significantly reduce the risk of these complications. Parents and caregivers should remain vigilant about monitoring symptoms and adhering to prescribed care plans.
Living with Patent Ductus Arteriosus
With advancements in medical technology and expertise, most individuals diagnosed with this condition can expect positive outcomes. Support from healthcare professionals, family members, and peer groups can make a substantial difference in managing the emotional and practical aspects of living with a congenital heart defect.
Emotional Well-Being
Children and adults with chronic health conditions may face unique psychological challenges. Encouraging open communication, providing reassurance, and seeking professional counseling when needed can foster resilience and improve quality of life.