Patellar tendinitis, commonly referred to as jumper’s knee, is a condition that affects the tendon connecting the kneecap to the shinbone. This overuse injury is prevalent among athletes who engage in sports requiring frequent jumping, such as basketball and volleyball. While the abbreviation PT is often used in medical contexts, we will explore this condition in detail without relying on abbreviations for clarity.
Understanding Patellar Tendinitis
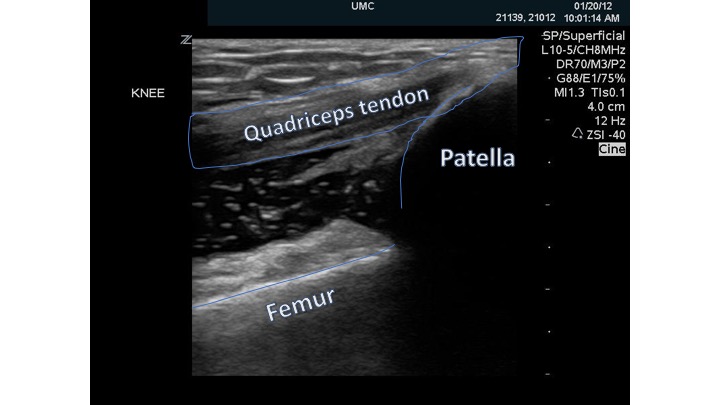
Patellar tendinitis occurs when the tendon that connects the kneecap to the shinbone becomes inflamed or irritated. This tendon plays a crucial role in allowing the knee to extend, making it essential for activities like running, jumping, and kicking. When this tendon is subjected to repetitive stress, small tears can develop, leading to pain and discomfort.
How It Differs from Other Knee Conditions
- Unlike arthritis, which involves joint inflammation, patellar tendinitis specifically targets the tendon.
- It is distinct from ligament injuries, which affect the structures stabilizing the knee joint.
- While conditions like bursitis involve fluid-filled sacs, patellar tendinitis focuses on the tendon itself.
Common Causes of Patellar Tendinitis
The development of patellar tendinitis is often linked to repetitive stress and overuse. Understanding its causes can help individuals take preventive measures and seek appropriate treatment.
Repetitive Stress and Overuse
Activities that require frequent jumping, running, or sudden changes in direction place significant strain on the tendon. Athletes involved in sports such as basketball, volleyball, soccer, and track and field are particularly susceptible. The repeated contraction of the quadriceps muscle during these activities pulls on the tendon, leading to microtears and eventual inflammation.
Poor Conditioning and Muscle Imbalance
Inadequate conditioning of the muscles around the knee can contribute to the development of patellar tendinitis. Weak quadriceps or hamstrings may fail to support the knee properly, increasing the load on the tendon. Additionally, muscle imbalances, where one group of muscles is stronger than the opposing group, can create uneven stress on the tendon.
Improper Technique and Equipment
Using incorrect techniques during physical activities can exacerbate stress on the tendon. For example, landing improperly after a jump or using footwear with inadequate support can increase the risk of developing patellar tendinitis. Similarly, playing on hard surfaces without proper cushioning can amplify the impact on the knees.
Age and Physical Condition
As people age, their tendons lose elasticity and become more prone to injury. Older adults who engage in high-impact activities may find themselves at greater risk. Furthermore, individuals with pre-existing conditions such as obesity or chronic illnesses may experience additional strain on their tendons, heightening the likelihood of developing patellar tendinitis.
Symptoms of Patellar Tendinitis
Recognizing the symptoms of patellar tendinitis is crucial for early diagnosis and treatment. The symptoms typically progress gradually and worsen over time if left untreated.
Pain Below the Kneecap
The most common symptom is pain located just below the kneecap. Initially, the pain may only occur during or after physical activity. As the condition progresses, the pain may become constant, even during daily activities like walking or climbing stairs.
Tenderness and Swelling
The affected area may feel tender to the touch, and some individuals may notice mild swelling around the tendon. This tenderness can make it uncomfortable to apply pressure to the knee, such as when kneeling or squatting.
Stiffness and Reduced Range of Motion
Individuals with patellar tendinitis may experience stiffness in the knee, especially after periods of inactivity, such as sitting for an extended time. This stiffness can limit the range of motion, making it difficult to fully extend or bend the knee.
Weakened Performance
Athletes may notice a decline in their performance due to pain and reduced strength in the affected leg. Activities that once felt effortless, such as jumping or sprinting, may become challenging and uncomfortable.
Diagnosis of Patellar Tendinitis
To diagnose patellar tendinitis, healthcare providers rely on a combination of physical examinations, patient history, and imaging tests. Accurate diagnosis ensures that individuals receive the appropriate treatment plan tailored to their needs.
Physical Examination
During a physical examination, a doctor will assess the knee for signs of tenderness, swelling, and pain. They may also ask the patient to perform specific movements to evaluate the range of motion and identify any limitations or discomfort.
Patient History
Understanding the patient’s history is essential for diagnosis. The doctor will inquire about the nature of the pain, its duration, and any activities that exacerbate or alleviate the symptoms. Information about the patient’s athletic involvement and training regimen can provide valuable insights into the potential causes of the condition.
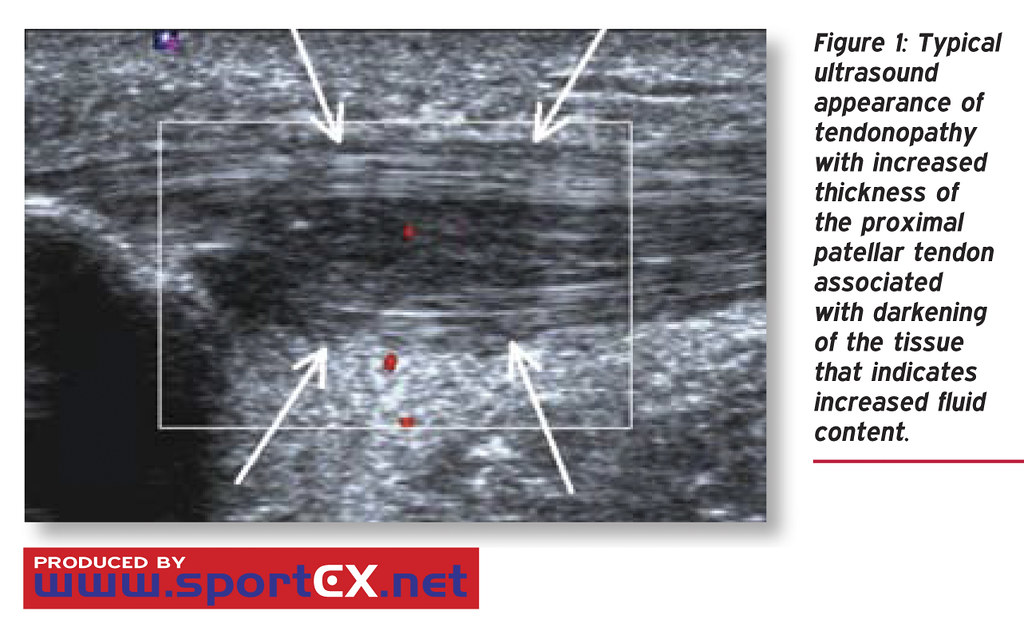
Imaging Tests
In some cases, imaging tests such as X-rays or magnetic resonance imaging may be recommended. While X-rays do not show soft tissues like tendons, they can help rule out other conditions, such as fractures. Magnetic resonance imaging provides detailed images of the tendon and surrounding structures, helping confirm the diagnosis and assess the severity of the injury.
Treatment Options for Patellar Tendinitis
Treating patellar tendinitis involves a combination of conservative measures and, in severe cases, surgical intervention. Early treatment can prevent the condition from worsening and promote faster recovery.
Rest and Activity Modification
One of the first steps in treating patellar tendinitis is reducing or modifying activities that aggravate the tendon. Resting the knee allows the tendon to heal, while avoiding high-impact activities prevents further damage. Cross-training with low-impact exercises, such as swimming or cycling, can help maintain fitness without straining the tendon.
Ice Therapy
Applying ice packs to the affected area can help reduce pain and swelling. Ice therapy is most effective when applied for 15 to 20 minutes several times a day, especially after physical activity.
Physical Therapy
Physical therapy plays a vital role in the rehabilitation process. A physical therapist can design a personalized exercise program to strengthen the muscles around the knee, improve flexibility, and correct muscle imbalances. Eccentric exercises, which focus on lengthening the muscle under tension, are particularly effective for tendon healing.
Medications
Over-the-counter pain relievers, such as ibuprofen or naproxen, can help manage pain and inflammation. In some cases, a doctor may prescribe stronger medications or recommend corticosteroid injections to reduce severe inflammation.
Orthotic Devices and Supportive Gear
Using orthotic devices, such as knee braces or straps, can provide additional support to the tendon and reduce strain during physical activity. Proper footwear with adequate cushioning and arch support is also essential for minimizing impact on the knees.
Surgical Intervention
In rare cases where conservative treatments fail to alleviate symptoms, surgery may be considered. Surgical options include removing damaged portions of the tendon or repairing tears. Surgery is typically reserved for individuals with chronic or severe cases of patellar tendinitis.
Preventive Measures for Patellar Tendinitis
Taking preventive measures can significantly reduce the risk of developing patellar tendinitis, especially for individuals involved in high-impact sports.
Proper Warm-Up and Stretching
Engaging in a thorough warm-up routine before physical activity prepares the muscles and tendons for exertion. Dynamic stretches, such as leg swings and lunges, can enhance flexibility and reduce the risk of injury.
Gradual Progression in Training
Avoiding sudden increases in intensity or duration of workouts allows the body to adapt gradually. Following a structured training plan with incremental progressions minimizes the risk of overuse injuries.
Strength and Conditioning Exercises
Incorporating strength training exercises for the quadriceps, hamstrings, and calves helps build resilience in the muscles supporting the knee. Balance and stability exercises can also improve overall joint function.
Listening to the Body
Paying attention to signs of pain or discomfort and addressing them promptly can prevent minor issues from escalating into serious injuries. Resting when necessary and seeking professional advice for persistent symptoms are essential practices for long-term knee health.