Parkinson’s Disease, often abbreviated as PD, is a progressive neurological disorder that affects millions of people worldwide. It primarily impacts movement and is characterized by a range of physical and cognitive symptoms. Despite its prevalence, many individuals remain unaware of the underlying causes, early warning signs, and available treatments for this condition. This article aims to provide a comprehensive overview of Parkinson’s Disease, shedding light on its fundamentals, symptoms, and the various approaches to managing it.
What is Parkinson’s Disease?
Parkinson’s Disease is a chronic and degenerative disorder of the central nervous system. It occurs when certain nerve cells in the brain, specifically those responsible for producing dopamine, begin to deteriorate or die. Dopamine is a neurotransmitter that plays a crucial role in regulating movement, mood, and other essential functions. When dopamine levels drop, it leads to the motor and non-motor symptoms associated with this disease.
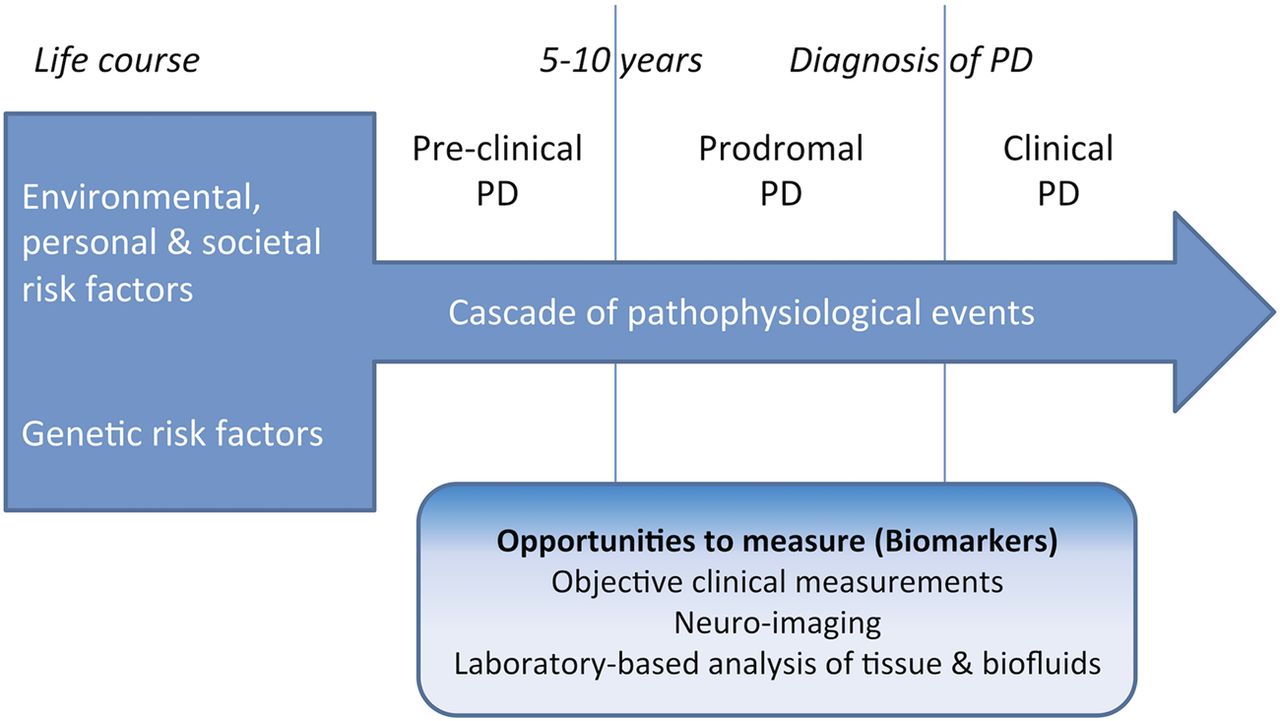
The exact cause of Parkinson’s remains unknown, but researchers believe that a combination of genetic and environmental factors may contribute to its development. While most cases occur sporadically, about 10 to 15 percent of cases are linked to specific genetic mutations. Environmental triggers such as exposure to toxins, head injuries, and aging are also considered potential risk factors.
How Common is Parkinson’s Disease?
Parkinson’s Disease is the second most common neurodegenerative disorder after Alzheimer’s Disease. It typically affects individuals over the age of 60, although younger people can also develop the condition, a phenomenon known as early-onset Parkinson’s. Men are slightly more likely to be diagnosed than women, and the prevalence of the disease increases with age.
Symptoms of Parkinson’s Disease
The symptoms of Parkinson’s Disease vary from person to person and tend to progress gradually over time. They can be broadly categorized into motor symptoms, which affect movement, and non-motor symptoms, which impact other aspects of health and well-being.
Motor Symptoms
Motor symptoms are often the most noticeable and debilitating aspects of Parkinson’s Disease. These include:
- Tremors: Involuntary shaking or trembling, usually starting in the hands, fingers, or limbs. Tremors are one of the earliest and most recognizable signs of the disease.
- Bradykinesia: Slowness of movement, making everyday tasks like walking, dressing, or eating increasingly difficult.
- Muscle Rigidity: Stiffness in the muscles, which can limit mobility and cause discomfort or pain.
- Postural Instability: Impaired balance and coordination, leading to an increased risk of falls.
- Shuffling Gait: A distinctive walking pattern characterized by short, shuffling steps and reduced arm swing.
Non-Motor Symptoms
In addition to motor symptoms, Parkinson’s Disease can also cause a wide range of non-motor issues, including:
- Cognitive Changes: Problems with memory, attention, and decision-making, which may eventually progress to dementia in some cases.
- Mood Disorders: Depression, anxiety, and apathy are common among individuals with Parkinson’s.
- Sleep Disturbances: Insomnia, restless leg syndrome, and REM sleep behavior disorder are frequently reported.
- Autonomic Dysfunction: Issues such as constipation, urinary problems, and fluctuations in blood pressure.
- Sensory Symptoms: Loss of smell, vision changes, and pain are also prevalent.
Diagnosing Parkinson’s Disease
Diagnosing Parkinson’s Disease can be challenging, as there is no single test to confirm its presence. Instead, healthcare providers rely on a combination of medical history, physical examinations, and symptom evaluation to make a diagnosis. Imaging tests, such as MRI or CT scans, are sometimes used to rule out other conditions that mimic Parkinson’s symptoms.
A key aspect of diagnosis involves observing the response to medications, particularly those that increase dopamine levels in the brain. If symptoms improve with such treatment, it strengthens the likelihood of a Parkinson’s diagnosis.
Early Warning Signs
Recognizing the early signs of Parkinson’s Disease is critical for timely intervention. Some subtle indicators include:
- Tremors in one hand or finger, especially when at rest.
- Changes in handwriting, such as smaller or cramped letters.
- Loss of sense of smell.
- Difficulty sleeping or acting out dreams during sleep.
- Stiffness or discomfort in the shoulders or hips.
Treatment Options for Parkinson’s Disease
While there is currently no cure for Parkinson’s Disease, several treatment options are available to manage symptoms and improve quality of life. The choice of treatment depends on the severity of symptoms, the individual’s overall health, and their personal preferences.
Medications
Medications are the cornerstone of Parkinson’s treatment and aim to replenish dopamine levels or mimic its effects in the brain. Commonly prescribed drugs include:
- Levodopa: Often considered the gold standard, this medication is converted into dopamine in the brain and helps alleviate motor symptoms.
- Dopamine Agonists: These drugs mimic the action of dopamine and can be used alone or in combination with levodopa.
- MAO-B Inhibitors: These medications prevent the breakdown of dopamine, extending its effects in the brain.
- COMT Inhibitors: Used alongside levodopa, these drugs help prolong its effectiveness.
Surgical Interventions
For individuals who do not respond well to medications or experience severe side effects, surgical options may be considered. Deep Brain Stimulation is one such procedure, where electrodes are implanted in specific areas of the brain to regulate abnormal neural activity. This treatment has been shown to reduce tremors, improve motor function, and decrease medication dependency.
Physical and Occupational Therapy
Physical therapy plays a vital role in managing Parkinson’s Disease by improving strength, flexibility, and balance. Occupational therapy focuses on helping individuals maintain independence in daily activities, such as dressing, cooking, and bathing. Both therapies can significantly enhance mobility and quality of life.
Lifestyle Modifications
Adopting a healthy lifestyle can complement medical treatments and promote overall well-being. Key strategies include:
- Exercise: Regular physical activity, such as walking, swimming, or yoga, can help improve motor function and reduce stiffness.
- Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports brain health and energy levels.
- Sleep Hygiene: Establishing a consistent sleep routine and addressing sleep disorders can improve restorative rest.
- Stress Management: Techniques such as mindfulness, meditation, and counseling can help cope with emotional challenges.
Emerging Research and Future Directions
Ongoing research into Parkinson’s Disease holds promise for better understanding its causes and developing innovative treatments. Scientists are exploring the potential of stem cell therapy, gene therapy, and neuroprotective agents to slow or halt disease progression. Advances in technology, such as wearable devices and artificial intelligence, are also being leveraged to monitor symptoms and personalize care.
The Role of Clinical Trials
Clinical trials are essential for testing new therapies and interventions. Participation in these studies not only contributes to scientific knowledge but also provides access to cutting-edge treatments that may not yet be widely available. Individuals interested in clinical trials should consult their healthcare provider for guidance and eligibility criteria.
Support Networks and Resources
Living with Parkinson’s Disease can be challenging, but support networks and resources are available to assist patients and their families. Support groups, educational programs, and advocacy organizations offer valuable information, emotional support, and opportunities to connect with others facing similar challenges.