Paraneoplastic syndromes, often abbreviated as PNS, refer to a group of rare disorders that arise as indirect effects of cancer. These syndromes occur when substances produced by tumors or the body’s immune response to cancer disrupt normal bodily functions. Unlike symptoms directly caused by the growth of a tumor, paraneoplastic syndromes affect distant organs and systems, making them challenging to diagnose and treat. This article explores the causes, symptoms, and treatment options for these complex conditions.
What Are Paraneoplastic Syndromes?
Paraneoplastic syndromes are not caused by the physical presence of a tumor but rather by substances secreted by the tumor or by the immune system’s reaction to the tumor. These syndromes can affect various parts of the body, including the nervous system, endocrine system, skin, and blood. They often appear before the underlying cancer is diagnosed, which can make identifying the root cause even more difficult.
While paraneoplastic syndromes are uncommon, they are significant because they can severely impact a patient’s quality of life. Understanding their mechanisms and manifestations is crucial for early detection and effective management.
Causes of Paraneoplastic Syndromes
The exact causes of paraneoplastic syndromes vary depending on the type of cancer and the affected organ system. However, two primary mechanisms are responsible for their development:
Hormonal or Substance Secretion by Tumors
- Tumors can produce hormones or other substances that mimic the actions of naturally occurring chemicals in the body. For example, certain lung cancers may secrete substances that mimic hormones produced by the adrenal glands, leading to imbalances in electrolytes or blood pressure.
- In some cases, tumors release cytokines or growth factors that interfere with normal cellular processes, causing systemic effects such as inflammation or abnormal tissue growth.
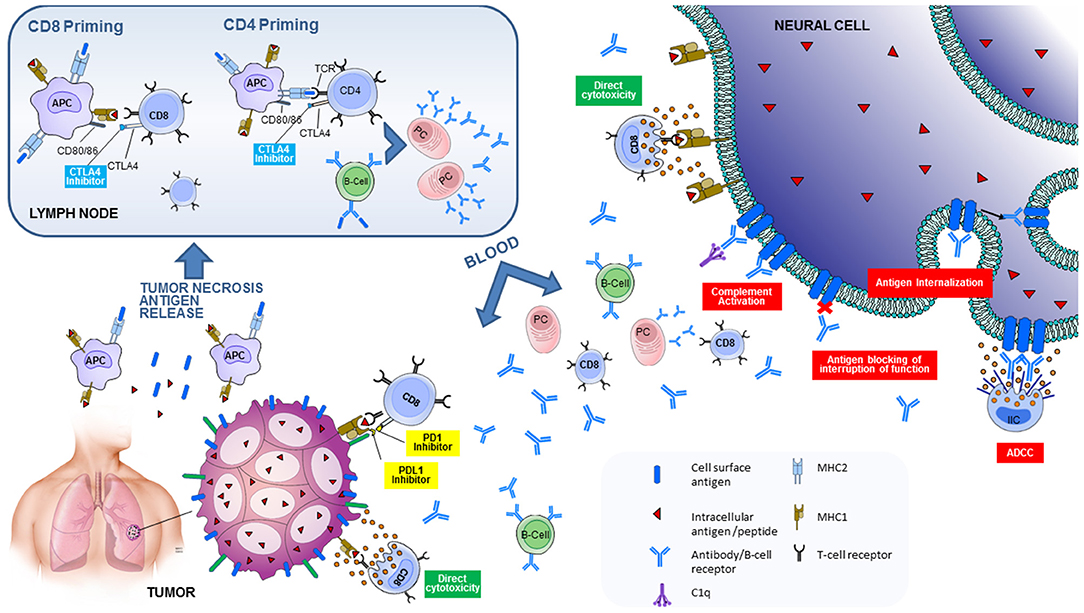
Immune System Response
- The immune system may mistakenly attack healthy tissues while trying to target the cancer cells. This autoimmune response can lead to damage in organs such as the brain, nerves, muscles, or skin.
- For instance, antibodies produced against tumor cells may cross-react with normal tissues, resulting in neurological symptoms like muscle weakness or cognitive impairment.
Common Types of Paraneoplastic Syndromes
There are numerous types of paraneoplastic syndromes, each affecting different parts of the body. Below are some of the most frequently observed categories:
Neurological Paraneoplastic Syndromes
- Lambert-Eaton Myasthenic Syndrome: This condition affects the neuromuscular junction, leading to muscle weakness, particularly in the legs and arms.
- Cerebellar Degeneration: Patients experience loss of coordination, difficulty walking, and slurred speech due to damage to the cerebellum.
- Encephalitis: Inflammation of the brain can result in confusion, memory problems, seizures, and changes in behavior.
Endocrine Paraneoplastic Syndromes
- Cushing Syndrome: Excessive production of cortisol-like substances by tumors can lead to weight gain, high blood pressure, and diabetes.
- Syndrome of Inappropriate Antidiuretic Hormone Secretion: This condition causes water retention, leading to low sodium levels in the blood and symptoms such as nausea, confusion, and seizures.
Dermatological Paraneoplastic Syndromes
- Acanthosis Nigricans: Characterized by dark, velvety patches of skin, often associated with cancers of the stomach or intestines.
- Dermatomyositis: An inflammatory condition marked by a rash and muscle weakness, commonly linked to ovarian or lung cancers.
Hematological Paraneoplastic Syndromes
- Erythrocytosis: Increased red blood cell production, which can thicken the blood and increase the risk of clotting.
- Thrombocytosis: Elevated platelet counts that may lead to excessive clotting or bleeding.
Symptoms of Paraneoplastic Syndromes
The symptoms of paraneoplastic syndromes depend on the specific type and the organs involved. Because these syndromes can mimic other diseases, they are often misdiagnosed initially. Some common symptoms include:
Neurological Symptoms
- Muscle weakness or paralysis
- Difficulty speaking or swallowing
- Loss of balance or coordination
- Seizures or memory loss
Endocrine Symptoms
- Unexplained weight gain or loss
- High blood pressure or irregular heartbeats
- Frequent urination or extreme thirst
Dermatological Symptoms
- Rashes or unusual skin discolorations
- Itching or swelling of the skin
Hematological Symptoms
- Fatigue or shortness of breath
- Bruising easily or unexplained bleeding
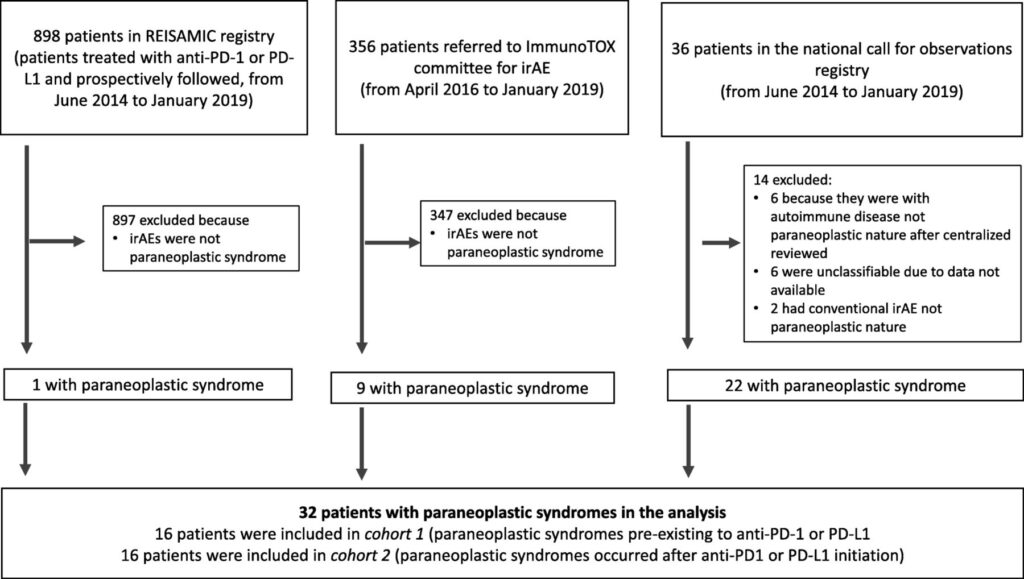
Diagnosis of Paraneoplastic Syndromes
Diagnosing paraneoplastic syndromes requires a comprehensive approach, as these conditions often present with vague or nonspecific symptoms. The following steps are typically involved:
Clinical Evaluation
- A thorough medical history and physical examination help identify potential signs of an underlying malignancy.
- Doctors look for patterns of symptoms that suggest a paraneoplastic origin rather than a primary disease.
Laboratory Tests
- Blood tests may reveal abnormal hormone levels, electrolyte imbalances, or the presence of specific autoantibodies associated with paraneoplastic syndromes.
- Imaging studies such as CT scans, MRI, or PET scans are used to locate tumors or assess organ damage.
Biopsy and Pathology
- In some cases, a biopsy of the affected tissue or suspected tumor is necessary to confirm the diagnosis.
- Pathological analysis helps determine whether the symptoms are indeed related to cancer.
Treatment Options for Paraneoplastic Syndromes
Treatment for paraneoplastic syndromes focuses on addressing both the underlying cancer and the symptoms caused by the syndrome itself. A multidisciplinary approach involving oncologists, neurologists, endocrinologists, and other specialists is often required.
Treating the Underlying Cancer
- Surgery: Removing the tumor can alleviate symptoms if the paraneoplastic syndrome is directly linked to the tumor’s activity.
- Chemotherapy and Radiation Therapy: These treatments aim to shrink or eliminate the cancer, potentially reducing the production of harmful substances or the immune response.
- Targeted Therapies: Medications designed to block specific pathways involved in tumor growth may also mitigate paraneoplastic effects.
Managing Symptoms
- Immunotherapy: Drugs that suppress the immune system, such as corticosteroids or intravenous immunoglobulin, can help control autoimmune reactions.
- Medications for Specific Symptoms: For example, anticonvulsants may be prescribed for seizures, while hormone replacement therapy can address endocrine imbalances.
- Physical and Occupational Therapy: These therapies assist patients with neurological symptoms in regaining strength and mobility.
Supportive Care
- Nutritional support and pain management are essential components of care for patients with paraneoplastic syndromes.
- Psychological counseling and support groups can help patients cope with the emotional toll of living with a chronic illness.
Prognosis and Ongoing Research
The prognosis for individuals with paraneoplastic syndromes varies widely depending on the type of syndrome, the stage of the underlying cancer, and the effectiveness of treatment. Early diagnosis and intervention improve outcomes significantly. Ongoing research aims to better understand the mechanisms behind these syndromes and develop targeted therapies to address their unique challenges.
Scientists are exploring the role of biomarkers and advanced imaging techniques to enhance diagnostic accuracy. Additionally, clinical trials are investigating novel treatments, including immunomodulatory drugs and gene therapies, to provide more personalized care for patients with paraneoplastic syndromes.