The pancreas is a vital organ located in the abdomen that plays a crucial role in digestion and blood sugar regulation. When this organ becomes inflamed, a condition known as pancreatitis occurs. Acute pancreatitis refers to sudden inflammation that can last for days, while chronic pancreatitis involves long-term damage and dysfunction of the pancreas. Both forms of this condition can significantly impact an individual’s health and quality of life. This article delves into the causes, symptoms, and treatments associated with pancreatitis to provide a comprehensive understanding of this medical condition.
What Is the Pancreas and What Does It Do?
The pancreas is a glandular organ situated behind the stomach, near the first part of the small intestine called the duodenum. It performs two primary functions: producing digestive enzymes and secreting hormones. The digestive enzymes help break down food in the intestines, while the hormones, such as insulin and glucagon, regulate blood sugar levels. When the pancreas becomes inflamed, its ability to perform these functions is compromised, leading to a host of complications.
How Does Pancreatitis Develop?
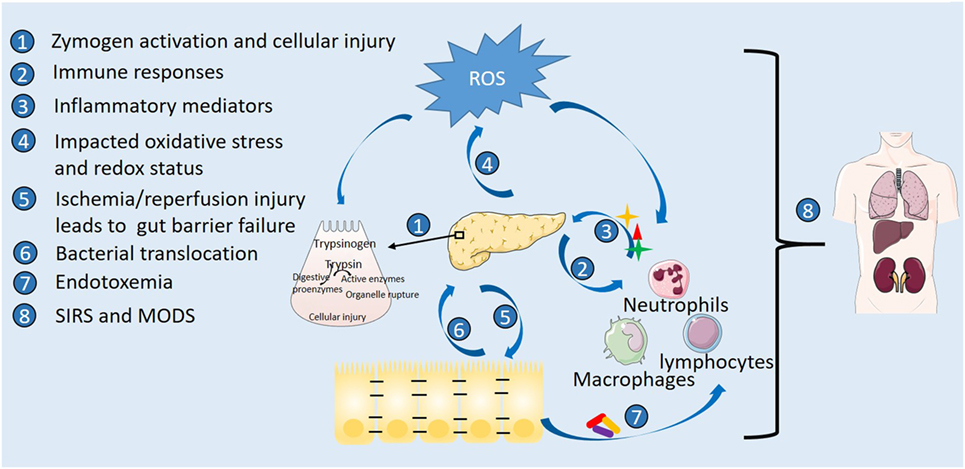
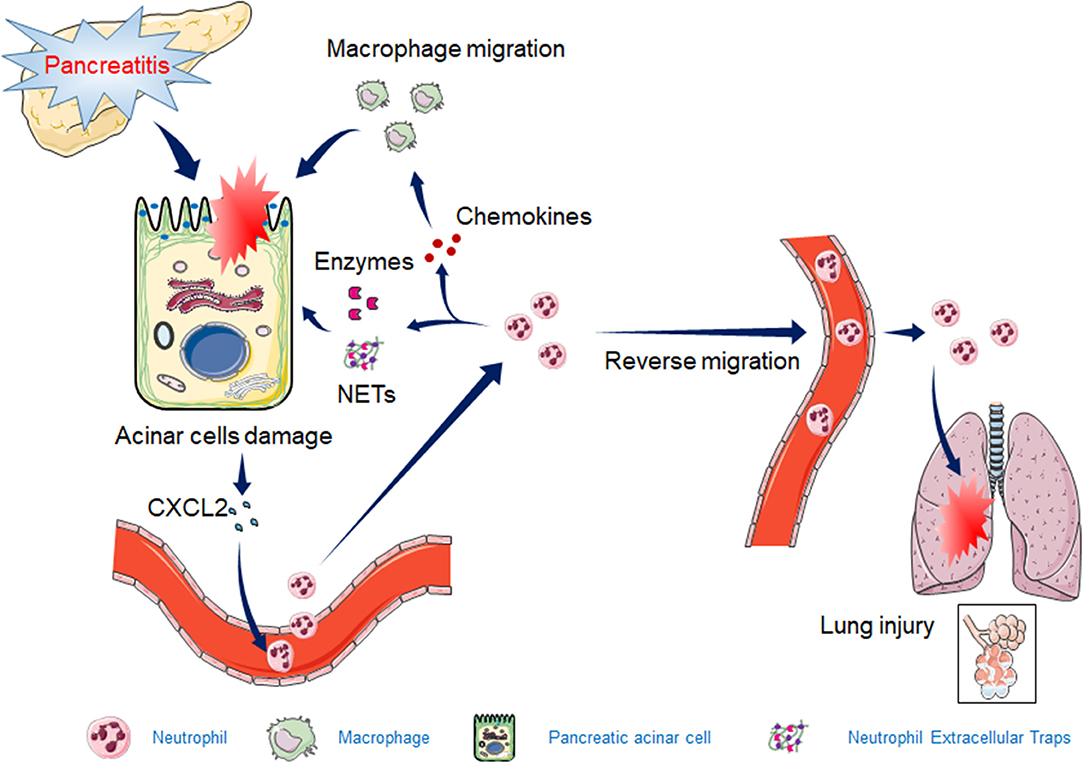
Pancreatitis occurs when the digestive enzymes produced by the pancreas become activated while still inside the organ. Normally, these enzymes are inactive until they reach the small intestine. However, in pancreatitis, they start digesting the pancreatic tissue itself, causing inflammation and damage. This process can be triggered by various factors, which will be explored in detail below.
Causes of Pancreatitis
There are several potential causes of pancreatitis, ranging from lifestyle factors to underlying medical conditions. Identifying the root cause is essential for effective treatment and prevention of recurrence.
Gallstones
Gallstones are one of the most common causes of acute pancreatitis. These hardened deposits form in the gallbladder and can block the ducts that connect the pancreas to the small intestine. When this happens, digestive enzymes back up into the pancreas, leading to inflammation.
Excessive Alcohol Consumption
Chronic alcohol use is another leading cause of both acute and chronic pancreatitis. Over time, alcohol can damage the cells of the pancreas, impair enzyme production, and lead to inflammation. Even short-term binge drinking can trigger acute episodes of pancreatitis in some individuals.
High Triglyceride Levels
Elevated levels of triglycerides, a type of fat found in the blood, can also contribute to pancreatitis. Extremely high levels of triglycerides can cause the formation of fatty deposits in the pancreas, increasing the risk of inflammation.
Trauma or Surgery
Injury to the abdomen, whether due to an accident or surgical procedure, can damage the pancreas and result in inflammation. Such cases are less common but should not be overlooked.
Medications
Certain medications have been linked to pancreatitis as a rare side effect. Examples include some antibiotics, diuretics, and immunosuppressive drugs. If you suspect your medication may be contributing to symptoms of pancreatitis, consult your healthcare provider immediately.
Genetic Factors
In some cases, genetic mutations can predispose individuals to pancreatitis. Hereditary pancreatitis is a rare condition caused by specific gene abnormalities that affect enzyme production and secretion.
Other Causes
- Infections, such as mumps or viral hepatitis
- Autoimmune disorders where the immune system mistakenly attacks the pancreas
- Pancreatic cancer or tumors obstructing the flow of enzymes
Symptoms of Pancreatitis
The symptoms of pancreatitis vary depending on whether it is acute or chronic. Recognizing these signs early can help prevent complications and ensure timely treatment.
Acute Pancreatitis Symptoms
Acute pancreatitis often presents suddenly and includes the following symptoms:
- Severe abdominal pain that radiates to the back
- Nausea and vomiting
- Fever and rapid pulse
- Tenderness in the abdomen upon touch
- Bloating and indigestion
If left untreated, acute pancreatitis can lead to serious complications such as infection, kidney failure, or respiratory problems.
Chronic Pancreatitis Symptoms
Chronic pancreatitis develops gradually over time and may present with milder symptoms initially. As the condition progresses, the following symptoms may occur:
- Persistent abdominal pain that worsens after eating
- Unintended weight loss due to malabsorption of nutrients
- Fatty stools resulting from poor digestion of fats
- Diabetes due to impaired insulin production
Individuals with chronic pancreatitis may experience periods of remission followed by flare-ups of symptoms.
Diagnosis of Pancreatitis
To diagnose pancreatitis, healthcare providers rely on a combination of physical examinations, laboratory tests, and imaging studies. Early diagnosis is critical to prevent further damage to the pancreas.
Physical Examination
A doctor will assess the patient’s symptoms, review their medical history, and perform a physical examination. They may check for abdominal tenderness, swelling, or signs of jaundice (yellowing of the skin and eyes).
Laboratory Tests
Blood tests are commonly used to detect elevated levels of pancreatic enzymes, such as amylase and lipase, which indicate inflammation. Other tests may evaluate liver function, calcium levels, and triglyceride concentrations.
Imaging Studies
Imaging techniques like ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI) provide detailed pictures of the pancreas. These tools help identify structural abnormalities, gallstones, or other obstructions contributing to the condition.
Treatment Options for Pancreatitis
The treatment approach for pancreatitis depends on the severity and underlying cause of the condition. While mild cases may resolve with conservative measures, severe cases often require hospitalization and intensive care.
Hospitalization and Supportive Care
For acute pancreatitis, patients are typically admitted to the hospital for monitoring and supportive care. This includes:
- Fasting to allow the pancreas to rest
- Intravenous fluids to prevent dehydration
- Pain management using medications
- Oxygen therapy if breathing difficulties arise
Addressing Underlying Causes
Treating the root cause of pancreatitis is essential to prevent recurrence. For example:
- Gallstone-related pancreatitis may require removal of the gallbladder through a procedure called cholecystectomy.
- Alcohol-induced pancreatitis necessitates complete abstinence from alcohol.
- High triglyceride levels can be managed through dietary changes and medications.
Enzyme Replacement Therapy
In chronic pancreatitis, the pancreas may no longer produce sufficient digestive enzymes. Enzyme replacement therapy involves taking oral supplements to aid digestion and improve nutrient absorption.
Surgical Interventions
In severe cases or when complications arise, surgery may be necessary. Procedures include draining fluid collections, removing damaged tissue, or bypassing blocked ducts to restore normal function.
Lifestyle Modifications
Making healthy lifestyle choices can reduce the risk of developing pancreatitis or experiencing recurrent episodes. Recommendations include:
- Adopting a low-fat diet rich in fruits, vegetables, and whole grains
- Limiting alcohol consumption or avoiding it altogether
- Maintaining a healthy weight through regular exercise
- Managing underlying conditions like diabetes or high cholesterol
Complications Associated With Pancreatitis
If left untreated or poorly managed, pancreatitis can lead to serious complications that affect multiple organs and systems in the body. Some potential complications include:
- Infection of the pancreas or surrounding tissues
- Pseudocysts, which are fluid-filled sacs that can rupture and cause internal bleeding
- Malnutrition due to impaired digestion and absorption of nutrients
- Diabetes resulting from damage to insulin-producing cells
- Kidney failure requiring dialysis or transplantation
Early intervention and adherence to treatment plans can minimize the risk of these complications and improve overall outcomes.