Pancreatic cancer, often abbreviated as PC, is a devastating disease that affects the pancreas, an organ located deep in the abdomen. It plays a critical role in digestion and regulating blood sugar levels. Despite advances in medical science, pancreatic cancer remains one of the most challenging cancers to diagnose and treat. This article delves into the causes, symptoms, diagnosis methods, and available treatments for this condition.
Understanding the Pancreas and Its Functions
The pancreas is a vital organ situated behind the stomach. It has two primary functions: producing enzymes that aid in digestion and releasing hormones like insulin and glucagon that help regulate blood sugar levels. When cancer develops in the pancreas, it disrupts these essential functions, leading to severe health complications.
What Is Pancreatic Cancer?
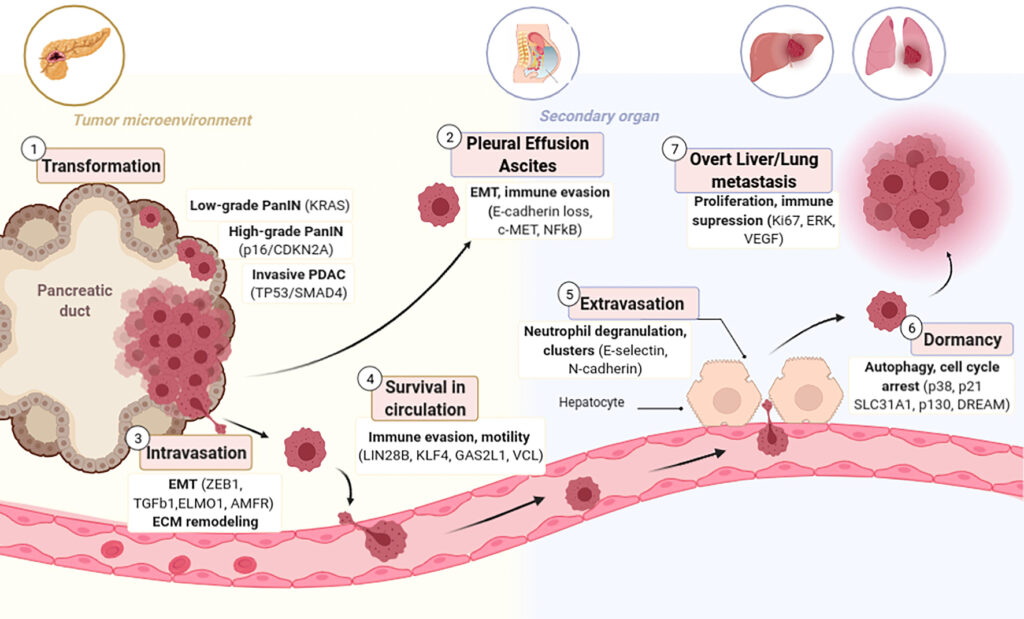
Pancreatic cancer occurs when abnormal cells in the pancreas grow uncontrollably, forming a tumor. These tumors can either be exocrine or endocrine, depending on the type of cells they originate from. Exocrine tumors are more common and typically develop in the ducts of the pancreas, while endocrine tumors arise from hormone-producing cells.
Causes of Pancreatic Cancer
The exact cause of pancreatic cancer is not fully understood, but several risk factors have been identified that increase the likelihood of developing the disease.
Genetic Factors
- Family History: Individuals with a family history of pancreatic cancer are at a higher risk. Certain inherited genetic mutations, such as those found in the BRCA1 and BRCA2 genes, also contribute to increased susceptibility.
- Rare Genetic Syndromes: Conditions like Lynch syndrome and Peutz-Jeghers syndrome are associated with a heightened risk of developing pancreatic cancer.
Lifestyle Factors
- Smoking: Smoking is one of the most significant risk factors for pancreatic cancer. It is estimated that smokers are two to three times more likely to develop the disease than nonsmokers.
- Obesity: Being overweight or obese increases the risk of pancreatic cancer. Fat tissue produces hormones and growth factors that may promote cancer development.
- Diet: A diet high in red meat and processed foods has been linked to an increased risk of pancreatic cancer.
Medical Conditions
- Diabetes: People with long-standing diabetes have a higher risk of developing pancreatic cancer. Conversely, new-onset diabetes can sometimes be an early sign of pancreatic cancer.
- Chronic Pancreatitis: Long-term inflammation of the pancreas increases the risk of cancerous changes in the organ.
Symptoms of Pancreatic Cancer
Pancreatic cancer is often called a “silent killer” because its symptoms are vague and nonspecific in the early stages. As the disease progresses, however, certain signs become more apparent.
Common Symptoms
- Abdominal Pain: Pain in the upper abdomen that radiates to the back is one of the most common symptoms of pancreatic cancer.
- Jaundice: Yellowing of the skin and eyes occurs when a tumor blocks the bile duct, preventing bile from reaching the intestines.
- Unexplained Weight Loss: Sudden and unexplained weight loss is a frequent symptom and often prompts individuals to seek medical attention.
- Loss of Appetite: Many patients report a reduced desire to eat, which contributes to weight loss.
Less Common Symptoms
- Nausea and Vomiting: These symptoms may occur if the tumor presses on the stomach or other nearby organs.
- Blood Clots: Some individuals with pancreatic cancer develop blood clots in the legs or lungs.
- New-Onset Diabetes: In some cases, pancreatic cancer leads to the development of diabetes due to the pancreas’s impaired ability to produce insulin.
Diagnosis of Pancreatic Cancer
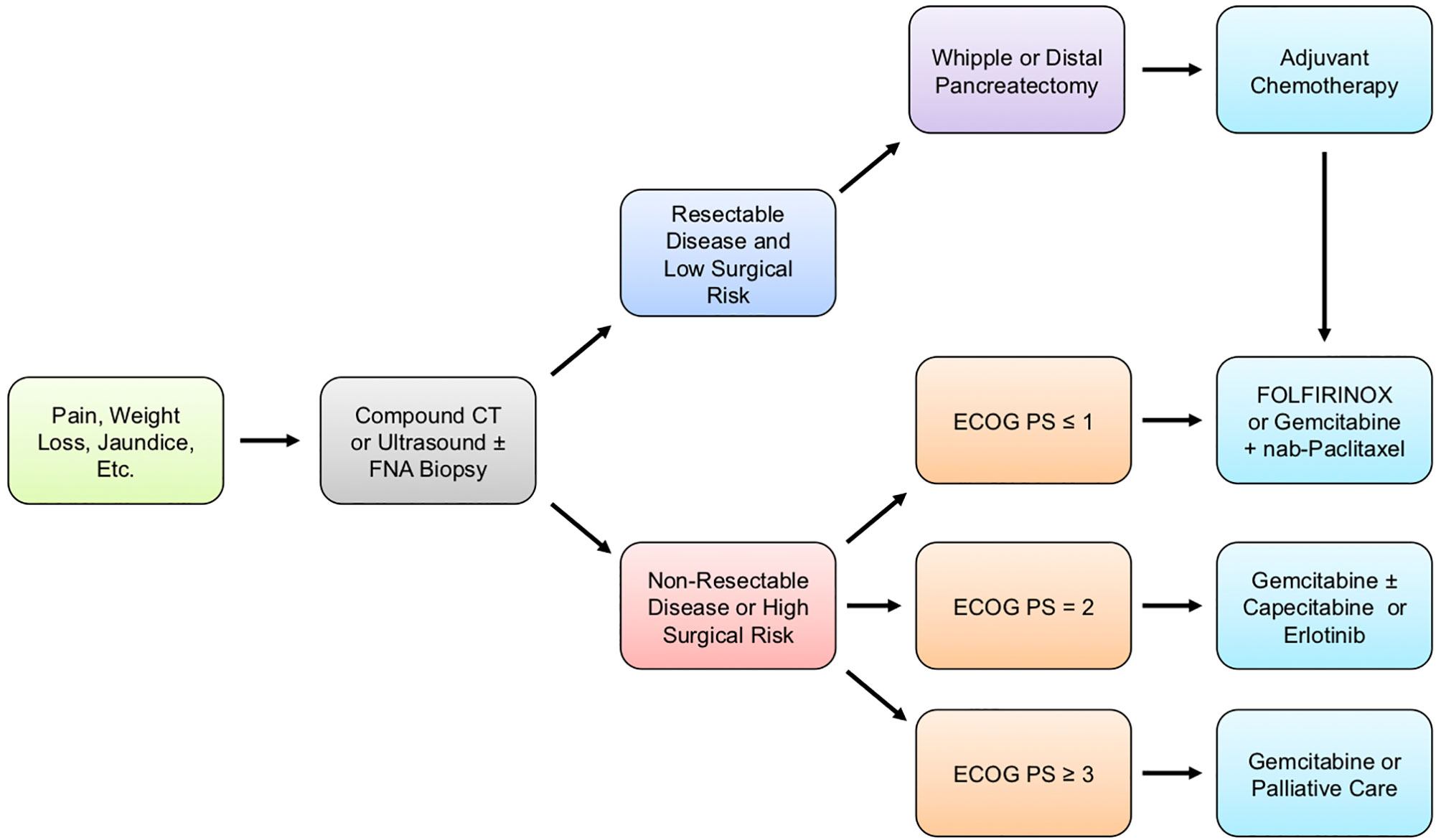
Diagnosing pancreatic cancer can be challenging because its symptoms often mimic those of other less serious conditions. Early detection is crucial for improving outcomes, but it is often delayed due to the nonspecific nature of the symptoms.
Initial Evaluation
When a patient presents with symptoms suggestive of pancreatic cancer, the doctor will begin with a thorough medical history and physical examination. The healthcare provider may ask about risk factors such as smoking, family history, and existing medical conditions.
Imaging Tests
- Computed Tomography Scan: A CT scan provides detailed images of the pancreas and surrounding structures, helping identify tumors and assess their size and location.
- Magnetic Resonance Imaging: MRI scans use magnetic fields to produce clear images of the pancreas and are particularly useful for evaluating soft tissues.
- Endoscopic Ultrasound: This procedure involves inserting a thin, flexible tube with an ultrasound probe into the digestive tract to obtain close-up images of the pancreas.
Biopsy
A biopsy is often necessary to confirm the presence of cancer. During this procedure, a small sample of tissue is removed from the pancreas and examined under a microscope. Biopsies can be performed using various techniques, including fine-needle aspiration guided by imaging.
Blood Tests
Blood tests alone cannot diagnose pancreatic cancer, but they can provide valuable information. For example, elevated levels of a protein called CA 19-9 are sometimes associated with pancreatic cancer, although this marker is not specific to the disease.
Treatment Options for Pancreatic Cancer
Treatment for pancreatic cancer depends on several factors, including the stage of the disease, the patient’s overall health, and personal preferences. While the prognosis for advanced pancreatic cancer remains poor, ongoing research continues to improve treatment options.
Surgery
Surgical removal of the tumor offers the best chance for a cure, but it is only possible if the cancer has not spread beyond the pancreas. The most common surgical procedures include:
- Whipple Procedure: Also known as a pancreaticoduodenectomy, this surgery removes the head of the pancreas, part of the small intestine, the gallbladder, and the bile duct.
- Distal Pancreatectomy: This procedure involves removing the tail and sometimes the body of the pancreas.
- Total Pancreatectomy: In rare cases, the entire pancreas may need to be removed.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. It is often used in combination with surgery or chemotherapy to shrink tumors before surgery or to eliminate remaining cancer cells afterward.
Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells. It is commonly used for advanced pancreatic cancer or when surgery is not an option. Chemotherapy can be administered orally or intravenously and is often combined with radiation therapy.
Targeted Therapy
Targeted therapy focuses on specific abnormalities within cancer cells that allow them to grow and survive. This approach is less harmful to normal cells compared to traditional chemotherapy and is often used for cancers with specific genetic mutations.
Immunotherapy
Immunotherapy harnesses the body’s immune system to fight cancer. While still under investigation for pancreatic cancer, immunotherapy holds promise for improving outcomes in certain patients.
Palliative Care
Palliative care focuses on relieving symptoms and improving quality of life for patients with advanced pancreatic cancer. This may include pain management, nutritional support, and addressing emotional and psychological needs.
Emerging Treatments and Research
Researchers are continually exploring new ways to detect and treat pancreatic cancer. Advances in genomics, personalized medicine, and novel drug therapies offer hope for better outcomes in the future.
- Vaccines: Experimental vaccines designed to stimulate the immune system against pancreatic cancer are currently being studied.
- Early Detection Biomarkers: Scientists are working to identify biomarkers that could lead to earlier diagnosis and improved survival rates.
- Combination Therapies: Combining different treatment modalities, such as chemotherapy, radiation, and immunotherapy, is being investigated to enhance effectiveness.