Osteoporosis, often abbreviated as OP, is a condition that affects millions of people worldwide. It weakens bones, making them fragile and more prone to fractures. This guide will delve into the intricacies of bone loss, exploring its causes, symptoms, risk factors, diagnosis, and treatment options. Whether you are seeking information for yourself or a loved one, this article aims to provide a comprehensive understanding of osteoporosis.
What Is Osteoporosis?
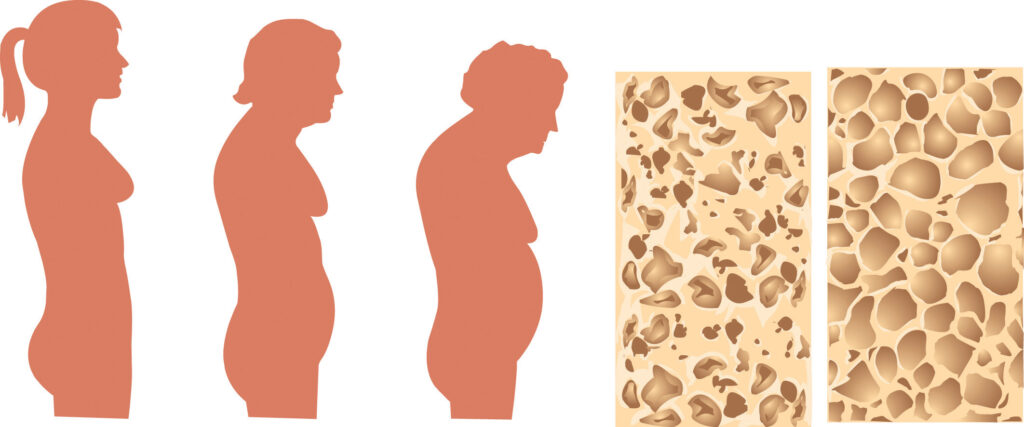
Osteoporosis is a progressive condition characterized by a decrease in bone density and quality. As a result, bones become porous, brittle, and more susceptible to fractures. The term “osteoporosis” literally means “porous bones.” While it is most commonly associated with aging, it can affect individuals of all ages, particularly postmenopausal women and older men.
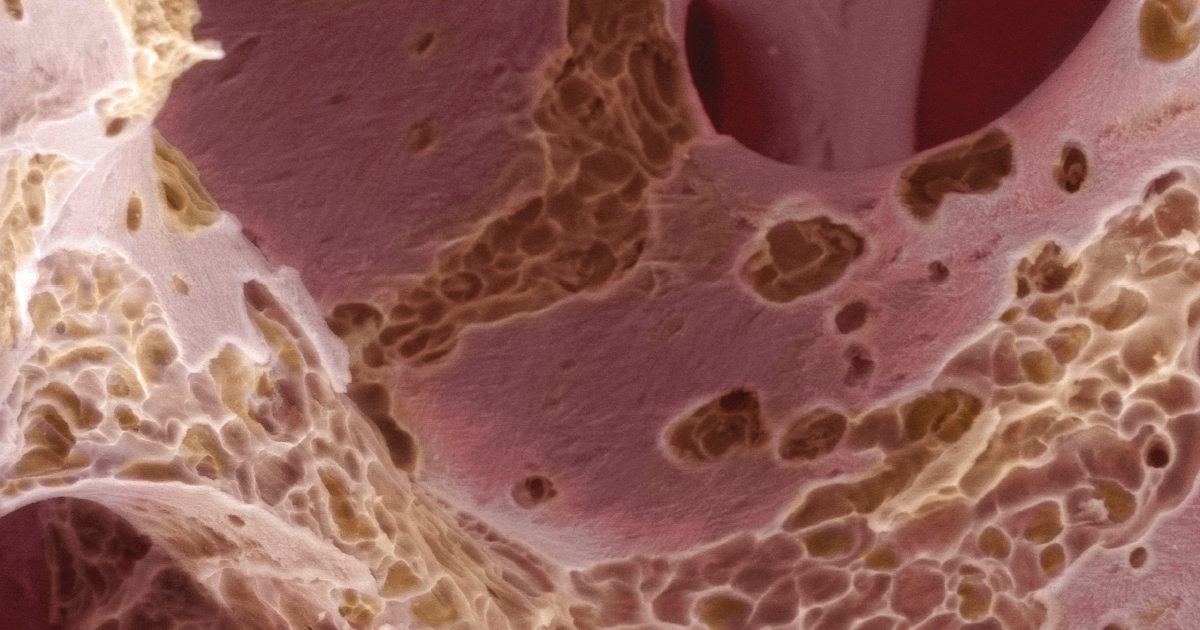
Bones are living tissues that undergo constant remodeling throughout life. In healthy individuals, old bone tissue is broken down and replaced with new bone tissue. However, in people with osteoporosis, the balance between bone formation and resorption is disrupted, leading to a net loss of bone mass.
The Anatomy of Bones
- Cortical Bone: The dense outer layer of bones that provides strength and protection.
- Trabecular Bone: The spongy inner layer of bones that contains bone marrow and contributes to bone flexibility.
In osteoporosis, both cortical and trabecular bones are affected, but trabecular bone tends to lose density more rapidly due to its higher turnover rate.
Causes of Osteoporosis
Osteoporosis can arise from a variety of factors, including genetic predisposition, hormonal changes, nutritional deficiencies, and lifestyle choices. Understanding these causes can help in prevention and early intervention.
Hormonal Changes
Hormones play a critical role in maintaining bone health. Estrogen, in particular, is essential for regulating bone density in women. During menopause, estrogen levels drop significantly, accelerating bone loss. Similarly, testosterone levels in men decline with age, contributing to bone thinning.
Nutritional Deficiencies
A diet lacking in essential nutrients can weaken bones over time. Key nutrients for bone health include:
- Calcium: A mineral that forms the structural component of bones.
- Vitamin D: Helps the body absorb calcium and supports bone growth.
- Protein: Provides the building blocks for bone tissue.
Inadequate intake of these nutrients can lead to decreased bone density and an increased risk of fractures.
Lifestyle Factors
Certain lifestyle habits can exacerbate bone loss. These include:
- Sedentary Lifestyle: Lack of physical activity can weaken bones and muscles.
- Smoking: Tobacco use interferes with bone healing and increases fracture risk.
- Excessive Alcohol Consumption: Heavy drinking can impair bone formation and increase the likelihood of falls.
Symptoms of Osteoporosis
Osteoporosis is often referred to as a “silent disease” because it typically progresses without noticeable symptoms until a fracture occurs. However, there are some subtle signs that may indicate bone loss:
- Loss of Height: Compression fractures in the spine can cause a gradual reduction in height.
- Stooped Posture: Also known as a dowager’s hump, this is caused by vertebral fractures.
- Back Pain: Fractures or collapsed vertebrae can lead to chronic pain.
- Frequent Fractures: Breaking bones easily, even from minor injuries, is a hallmark sign.
Risk Factors for Osteoporosis
While anyone can develop osteoporosis, certain factors increase the likelihood of developing the condition:
Age
Bone density naturally decreases with age, making older adults more vulnerable to osteoporosis.
Gender
Women are at a higher risk than men, especially after menopause, due to the rapid decline in estrogen levels.
Family History
A family history of osteoporosis or fractures can increase an individual’s susceptibility to the condition.
Medical Conditions
Certain health conditions, such as rheumatoid arthritis, hyperthyroidism, and gastrointestinal disorders, can contribute to bone loss.
Medications
Long-term use of medications like corticosteroids, anticonvulsants, and proton pump inhibitors can negatively impact bone health.
Diagnosing Osteoporosis
Early diagnosis is crucial for managing osteoporosis effectively. Healthcare providers use several methods to assess bone health and identify bone loss.
Bone Density Testing
The most common diagnostic tool is dual-energy X-ray absorptiometry, which measures bone mineral density. This test provides a T-score, comparing an individual’s bone density to that of a healthy young adult. A T-score of -2.5 or lower indicates osteoporosis.
Other Diagnostic Tools
- X-rays: Can detect fractures but are less effective for early-stage bone loss.
- Blood Tests: Measure levels of calcium, vitamin D, and other markers of bone metabolism.
- Fracture Risk Assessment Tool: Evaluates an individual’s risk of fractures based on various factors.
Treatment Options for Osteoporosis
While osteoporosis cannot be cured, there are several treatment strategies aimed at slowing bone loss, improving bone density, and reducing the risk of fractures.
Medications
Several types of medications are available to treat osteoporosis:
- Bisphosphonates: Help slow bone breakdown and are often the first line of treatment.
- Hormone Replacement Therapy: Replaces declining estrogen levels in postmenopausal women.
- Selective Estrogen Receptor Modulators: Mimic the effects of estrogen on bones without affecting other tissues.
- Anabolic Agents: Stimulate new bone formation and are used for severe cases.
Lifestyle Modifications
Making healthy lifestyle choices can significantly improve bone health:
- Exercise: Weight-bearing and resistance exercises strengthen bones and muscles.
- Balanced Diet: Consuming foods rich in calcium, vitamin D, and protein supports bone health.
- Fall Prevention: Removing tripping hazards and using assistive devices can reduce the risk of fractures.
Supplements
In cases where dietary intake is insufficient, supplements can help bridge the gap:
- Calcium Supplements: Ensure adequate intake for bone maintenance.
- Vitamin D Supplements: Enhance calcium absorption and support immune function.
Preventing Osteoporosis
Prevention is always better than cure, and adopting healthy habits early in life can reduce the risk of developing osteoporosis later on.
Building Strong Bones in Youth
Peak bone mass is achieved during adolescence and early adulthood. Encouraging children and young adults to engage in regular physical activity and consume a nutrient-rich diet can lay the foundation for strong bones.
Maintaining Bone Health in Adulthood
Even in adulthood, it is never too late to take steps to protect bone health. Regular exercise, a balanced diet, and avoiding harmful habits like smoking and excessive alcohol consumption can make a significant difference.
Regular Check-Ups
For individuals at high risk of osteoporosis, regular bone density screenings and consultations with healthcare providers can help monitor bone health and implement preventive measures.