Nonalcoholic fatty liver disease, commonly abbreviated as NAFLD, is a growing health concern worldwide. It refers to the accumulation of excess fat in the liver of individuals who consume little to no alcohol. While it often starts as a benign condition, it can progress to more severe liver damage if left untreated. This article explores the causes, symptoms, diagnosis, and care strategies for this increasingly common condition.
Understanding Nonalcoholic Fatty Liver Disease
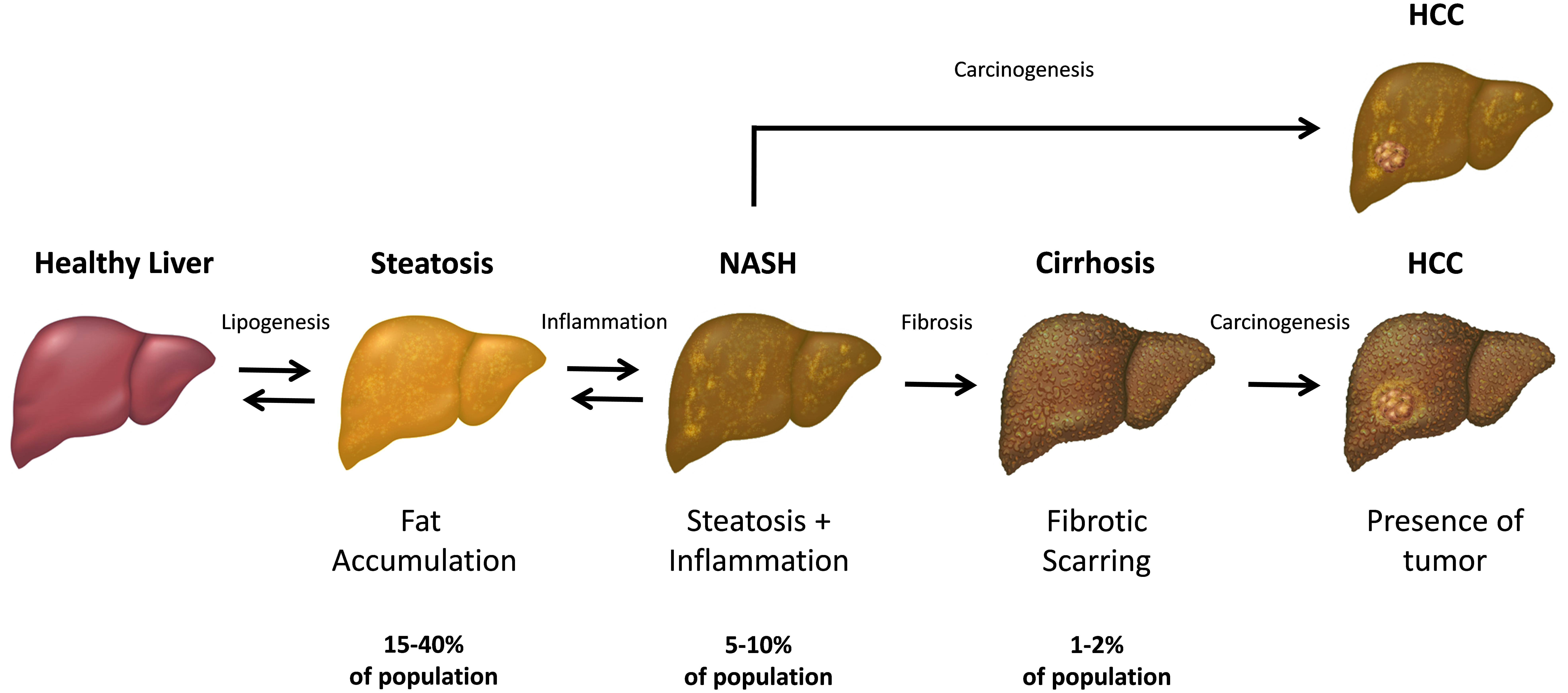
Nonalcoholic fatty liver disease is characterized by the buildup of fat in liver cells that is not related to excessive alcohol consumption. The liver plays a vital role in processing nutrients, filtering toxins, and producing essential proteins. When fat accumulates in the liver, it can disrupt these functions and lead to inflammation or scarring over time. There are two main types of this condition:
- Simple fatty liver: A mild form where fat builds up but does not cause significant inflammation or liver damage.
- Nonalcoholic steatohepatitis: A more severe form that involves liver inflammation and can lead to fibrosis (scarring) or cirrhosis (severe scarring).
Causes of Nonalcoholic Fatty Liver Disease
The exact cause of nonalcoholic fatty liver disease is not fully understood, but several factors contribute to its development. These include:
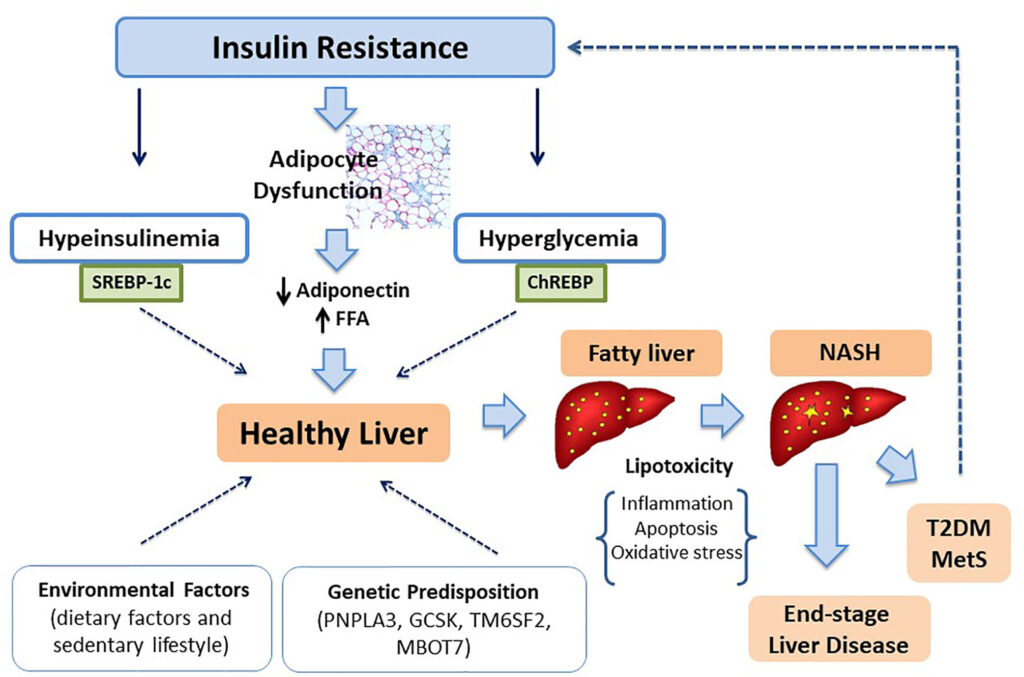
Obesity and Metabolic Syndrome
One of the primary risk factors for developing this condition is obesity. Excess body weight, particularly around the abdomen, increases the likelihood of fat accumulation in the liver. Metabolic syndrome, a cluster of conditions such as high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, also significantly raises the risk.
Insulin Resistance
Insulin resistance occurs when the body’s cells do not respond effectively to insulin, leading to elevated blood sugar levels. This condition is closely linked to nonalcoholic fatty liver disease, as it promotes fat storage in the liver and contributes to inflammation.
Unhealthy Diet
A diet high in refined carbohydrates, added sugars, and saturated fats can increase the risk of developing this condition. Consuming large amounts of sugary beverages, processed foods, and fried foods can overload the liver with fat.
Sedentary Lifestyle
Lack of physical activity is another contributing factor. Regular exercise helps burn fat and improves insulin sensitivity, reducing the risk of fat accumulation in the liver.
Genetic Factors
Some individuals may have a genetic predisposition to nonalcoholic fatty liver disease. Certain gene variations can affect how the body processes fat and responds to insulin, making some people more susceptible than others.
Other Medical Conditions
Conditions such as type 2 diabetes, high cholesterol, and polycystic ovary syndrome can also increase the risk of developing this liver condition. Additionally, certain medications and rapid weight loss can contribute to fat buildup in the liver.
Symptoms of Nonalcoholic Fatty Liver Disease
In its early stages, nonalcoholic fatty liver disease often does not cause noticeable symptoms. Many people are unaware they have the condition until it is detected during routine medical tests. However, as the disease progresses, some individuals may experience the following symptoms:
- Fatigue and weakness
- Discomfort or pain in the upper right abdomen
- Unexplained weight loss
- Swelling in the abdomen or legs
- Yellowing of the skin or eyes (jaundice)
It is important to note that these symptoms can also be associated with other health issues. Therefore, consulting a healthcare provider is essential for an accurate diagnosis.
Diagnosis of Nonalcoholic Fatty Liver Disease
Since nonalcoholic fatty liver disease often presents without symptoms, it is frequently discovered during routine blood tests or imaging studies conducted for other reasons. The diagnostic process typically involves the following steps:
Blood Tests
Blood tests can reveal elevated liver enzyme levels, which may indicate liver inflammation or damage. Common tests include alanine aminotransferase and aspartate aminotransferase measurements. However, normal enzyme levels do not rule out the presence of this condition.
Imaging Studies
Imaging techniques such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) can help detect fat accumulation in the liver. These noninvasive methods provide detailed images of the liver and surrounding structures.
Liver Biopsy
In some cases, a liver biopsy may be necessary to confirm the diagnosis and assess the extent of liver damage. During this procedure, a small sample of liver tissue is removed and examined under a microscope. While biopsies are considered the gold standard for diagnosis, they are invasive and carry some risks.
Noninvasive Tests
Recent advancements have led to the development of noninvasive tests, such as elastography, which measures liver stiffness to assess fibrosis. These tests are less risky and more convenient than traditional biopsies.
Care and Management of Nonalcoholic Fatty Liver Disease
While there is no specific medication to treat nonalcoholic fatty liver disease, lifestyle modifications and careful monitoring can help manage the condition and prevent progression. The following strategies are commonly recommended:
Weight Loss
Gradual weight loss is one of the most effective ways to reduce fat in the liver. Losing even five to ten percent of body weight can significantly improve liver health. However, rapid weight loss should be avoided, as it can worsen liver damage.
Healthy Diet
Adopting a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support liver health. Reducing intake of sugary beverages, processed foods, and saturated fats is crucial. The Mediterranean diet, which emphasizes plant-based foods and healthy fats like olive oil, has been shown to benefit individuals with this condition.
Regular Exercise
Physical activity plays a key role in managing nonalcoholic fatty liver disease. Engaging in at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, cycling, or swimming, can improve insulin sensitivity and reduce liver fat.
Management of Underlying Conditions
Controlling conditions such as type 2 diabetes, high cholesterol, and high blood pressure is essential for preventing further liver damage. Medications prescribed by a healthcare provider may be necessary to manage these conditions effectively.
Avoidance of Alcohol and Harmful Substances
Even though alcohol is not the cause of this condition, avoiding it altogether is recommended to prevent additional stress on the liver. Similarly, minimizing exposure to toxins and unnecessary medications can help protect liver function.
Regular Monitoring
Individuals diagnosed with nonalcoholic fatty liver disease should undergo regular check-ups to monitor liver health. Blood tests, imaging studies, and consultations with healthcare providers can help track the progression of the condition and guide treatment decisions.
Emerging Treatments
Research is ongoing to develop new treatments for this condition. Some promising approaches include medications targeting insulin resistance, inflammation, and fat metabolism. Clinical trials are exploring the potential benefits of vitamin E supplements, omega-3 fatty acids, and other therapies.
Preventing Nonalcoholic Fatty Liver Disease
Prevention is always better than cure, and adopting a healthy lifestyle can significantly reduce the risk of developing this condition. Key preventive measures include:
- Maintaining a healthy weight through a balanced diet and regular exercise
- Avoiding excessive consumption of sugary and processed foods
- Managing underlying health conditions such as diabetes and high cholesterol
- Staying physically active and incorporating movement into daily routines
- Limiting alcohol intake and avoiding harmful substances
By taking proactive steps, individuals can protect their liver health and reduce the likelihood of developing nonalcoholic fatty liver disease.