Neuromyelitis Optica, often abbreviated as NMO, is a rare autoimmune disorder that primarily affects the central nervous system. This condition targets the optic nerves and the spinal cord, leading to inflammation and damage that can result in significant neurological impairments. Unlike multiple sclerosis, which it is often mistaken for, this disease has distinct characteristics and requires specific approaches for diagnosis and treatment. In this article, we will explore the symptoms, diagnostic methods, and available treatments for this challenging condition.
Understanding Neuromyelitis Optica
Neuromyelitis Optica is a chronic condition that occurs when the immune system mistakenly attacks healthy cells in the central nervous system. The primary areas affected are the optic nerves, which transmit visual information from the eyes to the brain, and the spinal cord, which serves as a communication pathway between the brain and the rest of the body. This attack leads to inflammation, swelling, and damage to these critical structures, resulting in a range of debilitating symptoms.
Causes of Neuromyelitis Optica
The exact cause of this condition remains unknown, but researchers believe it involves a combination of genetic and environmental factors. One key factor is the presence of a specific antibody known as aquaporin-4, which plays a role in regulating water balance in the body. In individuals with this condition, the immune system produces antibodies that target aquaporin-4, leading to inflammation and damage in the central nervous system.
Other potential triggers include infections, stress, or exposure to certain environmental factors that may activate an abnormal immune response. While anyone can develop this condition, it is more commonly diagnosed in women and typically begins in adulthood.
Symptoms of Neuromyelitis Optica
The symptoms of this condition vary depending on which parts of the central nervous system are affected. However, there are two hallmark symptoms that are most commonly associated with this disorder:
Optic Neuritis
- Vision Loss: One of the earliest and most prominent symptoms is a sudden loss of vision in one or both eyes. This vision loss can range from mild blurriness to complete blindness.
- Eye Pain: Many individuals experience pain in or around the eyes, particularly when moving them. This pain can be severe and debilitating.
- Color Vision Changes: Colors may appear dull or washed out, making it difficult to distinguish between shades.
Transverse Myelitis
- Weakness or Paralysis: Inflammation of the spinal cord can lead to weakness or paralysis in the arms and legs. This symptom often develops rapidly and can severely impact mobility.
- Sensory Disturbances: Individuals may experience unusual sensations such as tingling, numbness, or burning along the spine and extremities.
- Bowel and Bladder Dysfunction: Loss of control over bowel and bladder functions is another common symptom, often accompanied by increased urgency or incontinence.
In addition to these hallmark symptoms, some individuals may also experience fatigue, muscle spasms, and difficulty coordinating movements. These symptoms can fluctuate in severity and may worsen during relapses.
Diagnosing Neuromyelitis Optica
Diagnosing this condition can be challenging due to its similarity to other neurological disorders, such as multiple sclerosis. However, advances in medical testing have improved the accuracy of diagnoses. The following steps are typically involved in identifying this condition:
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing this condition. During this process, healthcare providers review the patient’s medical history and conduct a detailed physical examination. They pay close attention to symptoms such as vision loss, weakness, and sensory disturbances, which may indicate involvement of the optic nerves or spinal cord.
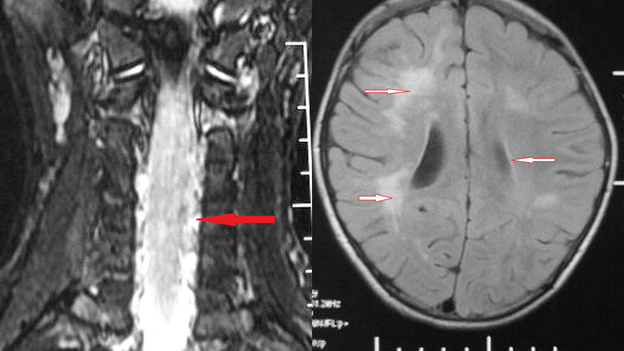
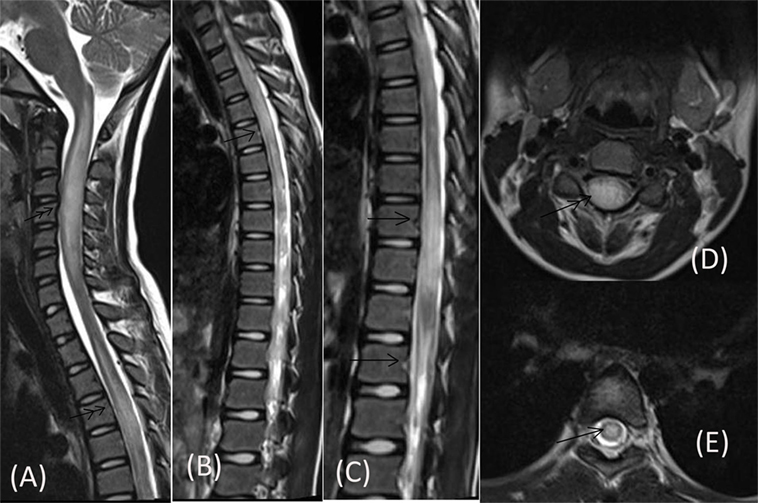
Magnetic Resonance Imaging
Magnetic resonance imaging, commonly referred to as MRI, is a critical tool in diagnosing this condition. MRI scans can reveal lesions or areas of inflammation in the optic nerves and spinal cord. Unlike multiple sclerosis, where lesions are typically scattered throughout the brain, this condition tends to produce longer, more extensive lesions in the spinal cord.
Laboratory Tests
Blood tests play a vital role in confirming the presence of aquaporin-4 antibodies, which are highly specific to this condition. Detecting these antibodies not only aids in diagnosis but also helps differentiate this condition from other similar disorders. In some cases, a lumbar puncture may be performed to analyze cerebrospinal fluid for signs of inflammation.
Differential Diagnosis
Because the symptoms of this condition overlap with those of other neurological disorders, ruling out alternative diagnoses is essential. Conditions such as multiple sclerosis, systemic lupus erythematosus, and infections of the central nervous system must be considered and excluded before a definitive diagnosis can be made.
Treatment Options for Neuromyelitis Optica
While there is currently no cure for this condition, several treatment options are available to manage symptoms, reduce relapses, and prevent long-term disability. The primary goals of treatment are to suppress the immune system’s abnormal response and minimize damage to the central nervous system.
Acute Treatment
During acute attacks, immediate treatment is necessary to reduce inflammation and prevent further damage. The following therapies are commonly used:
- Corticosteroids: High-dose intravenous corticosteroids, such as methylprednisolone, are administered to quickly reduce inflammation. These medications are typically given over several days and may be followed by a tapering dose of oral steroids.
- Plasma Exchange: If corticosteroids are ineffective, plasma exchange therapy may be recommended. This procedure involves removing harmful antibodies from the blood and replacing them with donor plasma.
Long-Term Management
To prevent relapses and slow disease progression, long-term immunosuppressive therapies are often prescribed. These treatments aim to modulate the immune system and reduce the frequency and severity of attacks. Common options include:
- Immunosuppressants: Medications such as azathioprine and mycophenolate mofetil are frequently used to suppress immune activity and prevent future attacks.
- Monoclonal Antibodies: Newer therapies, such as rituximab and eculizumab, target specific components of the immune system to reduce the risk of relapse. These treatments have shown promising results in clinical trials.
Symptom Management
In addition to addressing the underlying disease, managing symptoms is crucial for improving quality of life. Physical therapy, occupational therapy, and assistive devices can help individuals regain mobility and independence. Pain management strategies, including medications and nerve blocks, may also be employed to alleviate discomfort.
Lifestyle Modifications
Making certain lifestyle changes can complement medical treatments and enhance overall well-being. These include:
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, and whole grains can support immune health and reduce inflammation.
- Regular Exercise: Low-impact exercises, such as swimming or yoga, can improve strength, flexibility, and mental health.
- Stress Management: Techniques such as mindfulness meditation and deep breathing can help reduce stress, which may trigger relapses.
Emerging Research and Future Directions
Ongoing research into this condition continues to uncover new insights into its causes, mechanisms, and potential treatments. Scientists are exploring novel therapies that target specific pathways involved in the immune response, as well as biomarkers that could predict disease activity and treatment response. Clinical trials are also underway to evaluate the safety and efficacy of emerging drugs.
In addition to pharmacological advancements, efforts are being made to improve diagnostic tools and raise awareness about this condition among healthcare professionals and the general public. Early diagnosis and intervention remain critical for minimizing long-term complications and improving outcomes for affected individuals.
As our understanding of this condition evolves, so too does the hope for more effective treatments and, ultimately, a cure. By continuing to invest in research and education, we can work toward a future where individuals with this condition can live healthier, more fulfilling lives.