Neuroendocrine tumors, often abbreviated as NETs, are a rare and complex group of cancers that arise from neuroendocrine cells. These specialized cells have traits of both nerve cells and hormone-producing cells, allowing them to release hormones into the bloodstream in response to signals from the nervous system. Neuroendocrine tumors can occur in various parts of the body, with the most common locations being the gastrointestinal tract, lungs, and pancreas. This article provides an in-depth overview of these tumors, their types, symptoms, and care options.
Understanding Neuroendocrine Tumors
Neuroendocrine tumors develop when neuroendocrine cells grow uncontrollably, forming masses or tumors. These tumors can be benign or malignant, with malignant ones having the potential to spread to other parts of the body. What makes these tumors particularly challenging is their ability to produce hormones, which can lead to a wide range of symptoms depending on the type and location of the tumor.
The exact cause of neuroendocrine tumors is not fully understood, but certain genetic syndromes, such as multiple endocrine neoplasia, have been linked to an increased risk of developing these tumors. Additionally, factors like age, gender, and environmental influences may play a role in their development.
Types of Neuroendocrine Tumors
Neuroendocrine tumors are classified based on their location and behavior. Below are some of the most common types:
Gastrointestinal Neuroendocrine Tumors
- Carcinoid Tumors: These tumors typically occur in the stomach, small intestine, appendix, or rectum. Carcinoid tumors are often slow-growing and may not cause symptoms until they reach an advanced stage.
- Pancreatic Neuroendocrine Tumors: Also known as islet cell tumors, these tumors originate in the pancreas. They can be functional, meaning they produce hormones like insulin or gastrin, or nonfunctional, where they do not secrete hormones.
Lung Neuroendocrine Tumors
- Typical Carcinoid Tumors: These are the most common type of lung neuroendocrine tumors and tend to grow slowly.
- Atypical Carcinoid Tumors: These tumors are less common and tend to grow more aggressively than typical carcinoid tumors.
- Small Cell Lung Cancer: Although not always categorized under neuroendocrine tumors, this aggressive form of lung cancer shares some characteristics with neuroendocrine cells.
Other Types
- Medullary Thyroid Cancer: This type arises from the thyroid gland and is associated with hormone production.
- Merkel Cell Carcinoma: A rare and aggressive form of skin cancer that originates from neuroendocrine cells in the skin.
Symptoms of Neuroendocrine Tumors
The symptoms of neuroendocrine tumors vary widely depending on their location, size, and whether they are functional or nonfunctional. Functional tumors produce excess hormones, leading to specific syndromes, while nonfunctional tumors may not cause noticeable symptoms until they grow large enough to press on nearby organs.
Hormone-Related Symptoms
Functional neuroendocrine tumors can cause a variety of symptoms due to the overproduction of hormones. Some common examples include:
- Carcinoid Syndrome: This occurs when tumors in the gastrointestinal tract release serotonin and other substances into the bloodstream. Symptoms may include flushing, diarrhea, wheezing, and heart valve damage.
- Zollinger-Ellison Syndrome: Caused by tumors in the pancreas that produce excessive amounts of gastrin, leading to severe peptic ulcers and abdominal pain.
- Insulinomas: These tumors produce too much insulin, resulting in low blood sugar levels, which can cause confusion, weakness, and fainting.
Non-Hormonal Symptoms
Nonfunctional tumors may not produce hormones but can still cause symptoms due to their physical presence. These symptoms may include:
- Abdominal pain or discomfort
- Nausea and vomiting
- Bowel obstruction or changes in bowel habits
- A persistent cough or shortness of breath (if located in the lungs)
- Unexplained weight loss
Diagnosis of Neuroendocrine Tumors
Diagnosing neuroendocrine tumors can be challenging due to their rarity and diverse symptoms. A combination of imaging tests, laboratory tests, and biopsies is often required to confirm the diagnosis.
Imaging Tests
- Computed Tomography (CT) Scans: These scans provide detailed images of the body and can help identify the location and size of tumors.
- Magnetic Resonance Imaging (MRI): MRI scans are particularly useful for evaluating soft tissues and detecting tumors in the brain or spinal cord.
- Octreotide Scans: This specialized imaging test uses a radioactive substance to detect neuroendocrine tumors that have receptors for somatostatin, a hormone that regulates other hormones.
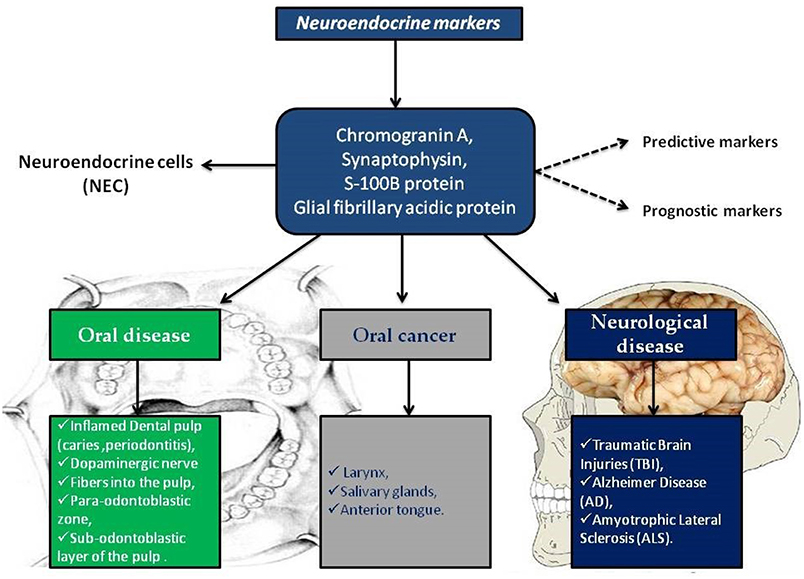
Laboratory Tests
- Blood Tests: These tests can measure hormone levels and other markers that may indicate the presence of a neuroendocrine tumor.
- Urine Tests: Analyzing urine samples can help detect elevated levels of certain substances, such as serotonin metabolites, which are associated with carcinoid syndrome.
Biopsy
A biopsy involves removing a small sample of tissue from the suspected tumor for examination under a microscope. This procedure is essential for confirming the diagnosis and determining the tumor’s grade and type.
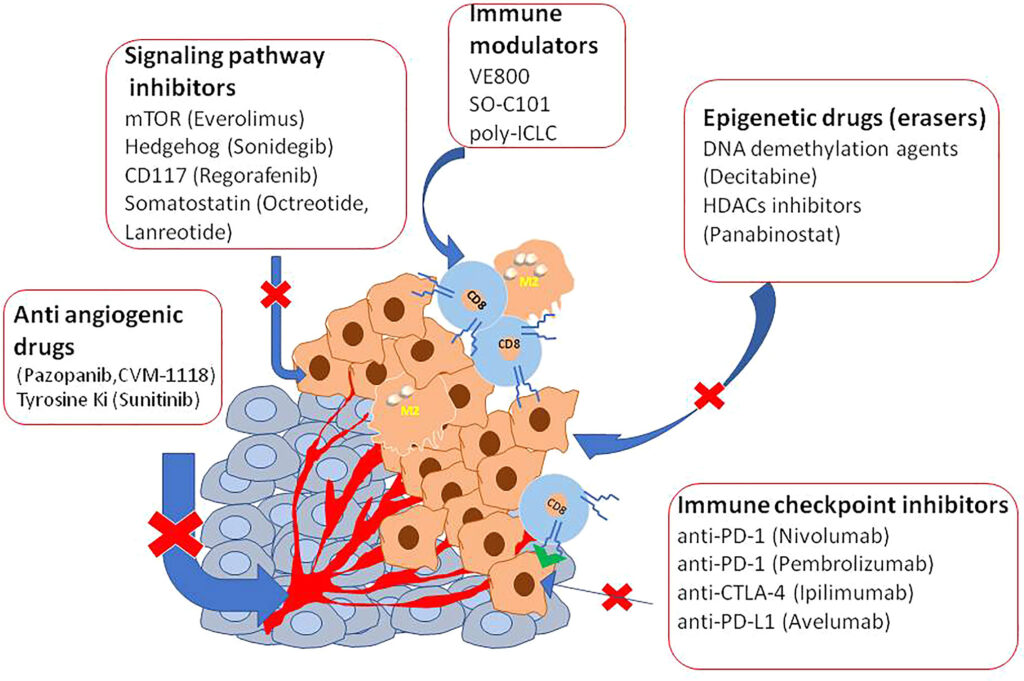
Treatment Options for Neuroendocrine Tumors
The treatment of neuroendocrine tumors depends on several factors, including the tumor’s location, size, grade, and whether it has spread to other parts of the body. A multidisciplinary approach involving oncologists, surgeons, and other specialists is often necessary to develop an effective treatment plan.
Surgery
Surgery is the primary treatment for localized neuroendocrine tumors. The goal is to remove the tumor completely, especially if it is confined to one area. In some cases, nearby lymph nodes may also need to be removed to ensure all cancerous cells are eliminated.
Medications
Several medications can help manage symptoms and slow the growth of neuroendocrine tumors:
- Somatostatin Analogs: These drugs mimic the effects of somatostatin, a hormone that inhibits the release of other hormones. They are often used to control symptoms of carcinoid syndrome and slow tumor growth.
- Targeted Therapy: Drugs like everolimus and sunitinib target specific pathways involved in tumor growth and are particularly effective for pancreatic neuroendocrine tumors.
- Chemotherapy: While not always effective for neuroendocrine tumors, chemotherapy may be used for aggressive or advanced cases.
Radiation Therapy
Radiation therapy uses high-energy particles to destroy cancer cells. It may be used to treat tumors that cannot be surgically removed or to relieve symptoms caused by tumors pressing on vital structures.
Peptide Receptor Radionuclide Therapy (PRRT)
This innovative treatment combines a radioactive substance with a peptide that targets neuroendocrine tumor cells. PRRT delivers radiation directly to the tumor, minimizing damage to surrounding healthy tissue.
Living with Neuroendocrine Tumors
Managing neuroendocrine tumors requires ongoing care and support. Patients often work closely with a team of healthcare providers to monitor their condition and adjust treatment plans as needed. Regular follow-up appointments, imaging tests, and blood work are essential to track the tumor’s progression and detect any recurrence early.
In addition to medical treatment, patients may benefit from lifestyle changes and supportive therapies to improve their quality of life. These may include dietary modifications, stress management techniques, and participation in support groups to connect with others facing similar challenges.
Dietary Considerations
For individuals with carcinoid syndrome or other hormone-related symptoms, dietary adjustments can help manage symptoms. For example, avoiding foods high in amines, such as aged cheeses and processed meats, may reduce flushing episodes. Consulting with a registered dietitian can provide personalized guidance based on individual needs.
Emotional and Psychological Support
A cancer diagnosis can be overwhelming, and emotional support is a critical component of care. Counseling, therapy, and support groups can help patients and their families cope with the emotional impact of living with neuroendocrine tumors. Many organizations also offer resources and educational materials to empower patients with knowledge about their condition.