Nephrogenic Systemic Fibrosis, often abbreviated as NSF, is a rare but serious condition that primarily affects individuals with severe kidney dysfunction. This progressive disorder leads to the thickening and hardening of the skin, along with potential involvement of internal organs. While it remains a rare occurrence, understanding its causes, symptoms, diagnosis, and treatment options is crucial for both patients and healthcare providers. In this article, we will explore each of these aspects in detail to provide a comprehensive overview of the condition.
What Causes Nephrogenic Systemic Fibrosis?
The exact cause of Nephrogenic Systemic Fibrosis remains somewhat elusive, but researchers have identified several key factors that contribute to its development. One of the most significant risk factors is exposure to gadolinium-based contrast agents, which are commonly used during magnetic resonance imaging scans. Gadolinium is a metal that enhances the clarity of MRI images, but in individuals with impaired kidney function, it can accumulate in the body and trigger the onset of this condition.
Risk Factors
- Severe Kidney Disease: People with advanced kidney disease, particularly those on dialysis or with a glomerular filtration rate below 15 mL/min/1.73 m², are at a higher risk.
- Exposure to Gadolinium-Based Contrast Agents: The use of these agents in imaging procedures has been strongly linked to the development of the condition.
- Inflammatory Conditions: Chronic inflammation or infections may exacerbate the risk of developing fibrotic changes in susceptible individuals.
- Acidosis and Hyperphosphatemia: Imbalances in the body’s acid-base levels and elevated phosphate levels can also play a role.
How Does It Develop?
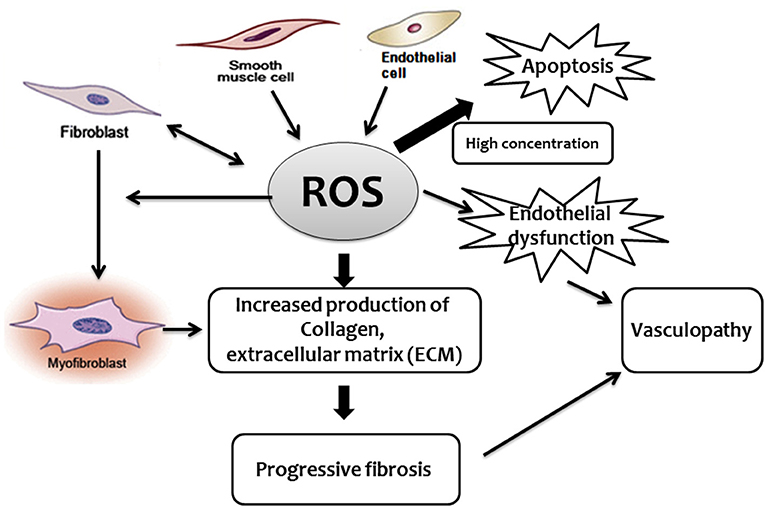
When gadolinium accumulates in the body due to impaired kidney function, it can lead to an abnormal immune response. This response triggers the activation of fibroblasts, cells responsible for producing collagen and other connective tissues. Over time, excessive collagen deposition results in the thickening and hardening of the skin and potentially affects internal organs such as the lungs, heart, and muscles.
Symptoms of Nephrogenic Systemic Fibrosis
The symptoms of this condition can vary widely depending on the severity of the disease and the organs involved. Initially, the changes may be subtle, but as the disease progresses, they become more pronounced and debilitating.
Skin-Related Symptoms
- Thickened Skin: One of the hallmark signs is the development of hardened, tight skin, often starting in the extremities like the legs and arms.
- Swelling: Affected areas may exhibit swelling, which can make movement difficult.
- Red or Dark Patches: Discoloration of the skin, appearing as red or dark patches, is common.
- Burning or Itching Sensation: Patients often report discomfort, including burning or itching sensations in the affected areas.
Systemic Symptoms
- Muscle Weakness: As the condition progresses, muscle weakness and joint stiffness may occur, limiting mobility.
- Organ Involvement: Internal organs such as the lungs, heart, and liver may also be affected, leading to complications like shortness of breath, heart failure, or liver dysfunction.
- Pain: Many individuals experience chronic pain, particularly in the joints and muscles.
Progression of Symptoms
The progression of symptoms can be rapid or gradual, depending on the individual. In some cases, the disease stabilizes after a period of worsening, while in others, it continues to advance, leading to significant disability.
Diagnosing Nephrogenic Systemic Fibrosis
Diagnosing this condition requires a thorough evaluation by healthcare professionals. Since the symptoms can mimic other diseases, a combination of clinical assessment, imaging studies, and laboratory tests is often necessary to confirm the diagnosis.
Clinical Evaluation
A detailed medical history and physical examination are the first steps in diagnosing the condition. Physicians will look for characteristic skin changes, assess kidney function, and inquire about any recent exposure to gadolinium-based contrast agents.
Biopsy
A skin biopsy is one of the most definitive diagnostic tools. During this procedure, a small sample of affected skin is removed and examined under a microscope. The presence of thickened collagen bundles and specific cellular changes can help confirm the diagnosis.
Imaging Studies
Magnetic resonance imaging or computed tomography scans may be used to evaluate the extent of tissue involvement. These imaging techniques can also help rule out other conditions that may present with similar symptoms.
Laboratory Tests
Blood tests to assess kidney function and detect markers of inflammation or fibrosis may also be conducted. Additionally, testing for gadolinium levels in the blood or urine can provide further evidence of exposure to gadolinium-based contrast agents.
Treatment Options for Nephrogenic Systemic Fibrosis
Currently, there is no cure for this condition, but various treatment strategies aim to manage symptoms, slow disease progression, and improve quality of life. The approach to treatment depends on the severity of the disease and the organs involved.
Improving Kidney Function
Since impaired kidney function is a major risk factor, improving renal health is a priority. For some patients, kidney transplantation may offer relief, as restoring normal kidney function can help eliminate gadolinium from the body and halt disease progression.
Medications
- Immunosuppressive Drugs: Medications like corticosteroids or immunosuppressants may be prescribed to reduce inflammation and modulate the immune response.
- Phototherapy: Ultraviolet light therapy has shown promise in some cases, helping to soften the skin and alleviate symptoms.
- Pain Management: Pain-relieving medications, including nonsteroidal anti-inflammatory drugs or opioids, may be used to manage chronic pain.
Physical Therapy
Physical therapy plays a crucial role in maintaining mobility and preventing joint stiffness. A tailored exercise program can help patients retain flexibility and improve their overall quality of life.
Supportive Care
Managing complications such as heart or lung involvement may require specialized care. Collaboration with a multidisciplinary team, including nephrologists, dermatologists, and rheumatologists, is essential for comprehensive management.
Preventive Measures
Preventing the condition is far more effective than treating it. Healthcare providers should carefully evaluate the need for gadolinium-based contrast agents in patients with kidney disease and consider alternative imaging methods when possible. Additionally, monitoring kidney function regularly and addressing underlying health issues can reduce the risk of developing this condition.
Ongoing Research and Future Directions
Research into this condition is ongoing, with scientists striving to better understand its mechanisms and develop targeted therapies. Advances in imaging technology and the development of safer contrast agents hold promise for reducing the incidence of this condition in the future. Clinical trials exploring new treatment options, including novel medications and regenerative therapies, are also underway.
Patient Advocacy and Awareness
Raising awareness about this condition among both healthcare providers and patients is critical. Patient advocacy groups play a vital role in supporting individuals affected by the condition and promoting research efforts. By fostering collaboration between researchers, clinicians, and patients, progress can be made toward better outcomes for those living with this challenging disease.