Muscular dystrophy, often abbreviated as MD, refers to a group of genetic disorders that cause progressive weakness and loss of muscle mass. These conditions are caused by mutations in genes responsible for the structure and function of muscles. While there is currently no cure for muscular dystrophy, ongoing research and advancements in medical science have led to improved management strategies and treatments that can help improve the quality of life for those affected. This article will explore the different types of muscular dystrophy, their causes, symptoms, and available treatments.
Understanding Muscular Dystrophy
Muscular dystrophy is not a single disorder but rather a collection of diseases that share similar characteristics. Each type of muscular dystrophy affects specific muscle groups and progresses at varying rates. The severity of symptoms and the age of onset can differ significantly depending on the type of muscular dystrophy an individual has.
What Happens in Muscular Dystrophy?
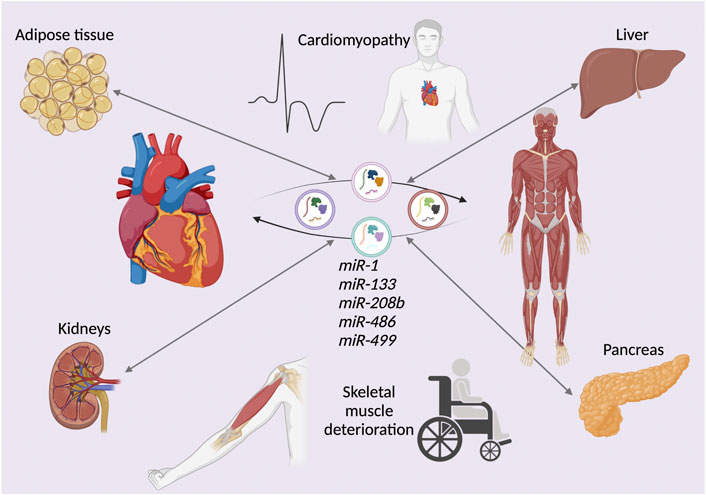
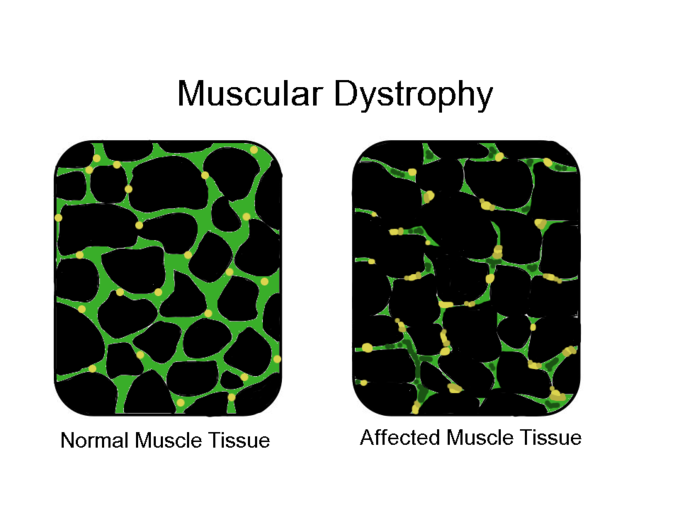
In individuals with muscular dystrophy, the body is unable to produce certain proteins that are essential for maintaining healthy muscle fibers. Over time, this leads to the degeneration of muscle tissue, which is replaced by fat and connective tissue. As a result, the muscles become weaker and less functional, making it difficult for individuals to perform everyday activities.
Types of Muscular Dystrophy
There are several types of muscular dystrophy, each with its own unique characteristics. Below is an overview of some of the most common forms:
Duchenne Muscular Dystrophy
- Onset: Typically begins in early childhood, usually between ages two and five.
- Affected Population: Primarily affects boys, although girls can be carriers of the gene mutation.
- Symptoms: Difficulty walking, frequent falls, muscle stiffness, and progressive loss of mobility. By adolescence, most individuals require a wheelchair.
Becker Muscular Dystrophy
- Onset: Symptoms usually appear later than in Duchenne muscular dystrophy, often during late childhood or adolescence.
- Affected Population: Also primarily affects males.
- Symptoms: Similar to Duchenne muscular dystrophy but progresses more slowly. Muscle weakness typically begins in the hips and thighs.
Myotonic Muscular Dystrophy
- Onset: Can occur at any age, including adulthood.
- Affected Population: Affects both men and women equally.
- Symptoms: Characterized by prolonged muscle contractions and difficulty relaxing muscles after use. Other symptoms include muscle weakness, cataracts, and heart problems.
Limb-Girdle Muscular Dystrophy
- Onset: Usually begins in late childhood or early adulthood.
- Affected Population: Affects both men and women.
- Symptoms: Weakness and wasting of muscles in the shoulders and hips. Individuals may experience difficulty lifting objects or climbing stairs.
Facioscapulohumeral Muscular Dystrophy
- Onset: Symptoms often appear during adolescence or early adulthood.
- Affected Population: Affects both men and women.
- Symptoms: Weakness in facial muscles, shoulders, and upper arms. Some individuals may also experience hearing loss or abnormalities in the retina.
Causes of Muscular Dystrophy
Muscular dystrophy is caused by genetic mutations that interfere with the production of proteins necessary for muscle health. These mutations can be inherited from one or both parents, or they can occur spontaneously in an individual without a family history of the condition.
Inherited Mutations
In many cases, muscular dystrophy is passed down through families. The inheritance pattern depends on the specific type of muscular dystrophy:
- X-Linked Recessive Inheritance: Seen in Duchenne and Becker muscular dystrophy. Since the mutated gene is located on the X chromosome, the condition primarily affects males.
- Autosomal Dominant Inheritance: Seen in myotonic and facioscapulohumeral muscular dystrophy. Only one copy of the mutated gene is needed to develop the condition.
- Autosomal Recessive Inheritance: Seen in limb-girdle muscular dystrophy. Two copies of the mutated gene (one from each parent) are required for the condition to manifest.
Spontaneous Mutations
In some cases, muscular dystrophy occurs due to a spontaneous mutation in the genes. This means that the condition is not inherited from either parent but arises as a new genetic change in the affected individual.
Symptoms of Muscular Dystrophy
The symptoms of muscular dystrophy vary depending on the type and severity of the condition. However, there are some common signs and symptoms that are often observed:
- Frequent falls and difficulty getting up from a sitting or lying position.
- Progressive muscle weakness, often starting in specific areas such as the legs, hips, or shoulders.
- Difficulty walking, running, or jumping.
- Delayed motor skills development in children.
- Waddling gait or walking on the toes.
- Pain and stiffness in muscles and joints.
- Respiratory difficulties due to weakened chest muscles.
- Cardiac complications, such as arrhythmias or heart failure, in certain types of muscular dystrophy.
Age of Onset and Progression
The age at which symptoms appear and the rate at which the condition progresses can vary widely. For example, Duchenne muscular dystrophy typically begins in early childhood and progresses rapidly, while myotonic muscular dystrophy may not manifest until adulthood and progresses more slowly.
Treatments for Muscular Dystrophy
While there is currently no cure for muscular dystrophy, various treatments and therapies can help manage symptoms, slow disease progression, and improve quality of life. Treatment plans are tailored to the specific needs of each individual and may involve a combination of approaches.
Medications
- Corticosteroids: These medications can help improve muscle strength and delay the progression of muscle weakness. However, long-term use may have side effects such as weight gain and bone thinning.
- Heart Medications: For individuals with cardiac complications, medications such as beta-blockers or ACE inhibitors may be prescribed to manage heart function.
- Gene Therapy: Emerging treatments aim to correct the underlying genetic mutations responsible for muscular dystrophy. While still largely experimental, gene therapy holds promise for future treatment options.
Physical and Occupational Therapy
Physical therapy plays a crucial role in maintaining muscle function and preventing joint contractures. Therapists work with individuals to develop exercise programs that focus on stretching, strengthening, and improving mobility. Occupational therapy helps individuals adapt to daily living challenges by teaching them techniques and providing assistive devices to enhance independence.
Assistive Devices
As muscular dystrophy progresses, individuals may require assistive devices to maintain mobility and independence. These devices include:
- Braces or orthotics to support weak muscles and joints.
- Wheelchairs or scooters for individuals who have difficulty walking.
- Respiratory aids such as ventilators or cough-assist devices for those with breathing difficulties.
Surgical Interventions
In some cases, surgery may be necessary to address complications associated with muscular dystrophy. For example:
- Scoliosis Surgery: To correct spinal curvature caused by weakened back muscles.
- Tendon Release Surgery: To alleviate joint contractures and improve range of motion.
Supportive Care
Beyond medical treatments, supportive care is essential for managing muscular dystrophy. This includes:
- Nutritional counseling to ensure proper nutrition and prevent obesity, which can exacerbate symptoms.
- Psychological support to address emotional and mental health challenges associated with living with a chronic condition.
- Regular monitoring by a multidisciplinary team of healthcare professionals, including neurologists, cardiologists, pulmonologists, and physical therapists.
Living with Muscular Dystrophy
Living with muscular dystrophy can be challenging, but with the right support and resources, individuals can lead fulfilling lives. Education, advocacy, and community involvement play important roles in empowering those affected by the condition and raising awareness about the need for continued research and innovation.