Multiple Sclerosis, often abbreviated as MS, is a chronic autoimmune condition that affects the central nervous system. This includes the brain, spinal cord, and optic nerves. It is characterized by an immune system malfunction where the body mistakenly attacks its own protective nerve coverings. These attacks disrupt communication between the brain and the rest of the body, leading to a wide range of symptoms. In this article, we will explore the disease in detail, understand its potential triggers, and discuss various management options available for those living with this condition.
What is Multiple Sclerosis?
Multiple Sclerosis is a complex neurological disorder that impacts millions of people worldwide. The term “sclerosis” refers to the scarring or hardening of tissue, which occurs when the immune system damages the myelin sheath—the protective layer surrounding nerve fibers. This damage leads to inflammation and the formation of scar tissue, making it difficult for the nervous system to transmit signals efficiently.
Symptoms of Multiple Sclerosis
The symptoms of this condition vary widely from person to person and depend on the location and extent of nerve damage. Some common symptoms include:
- Fatigue
- Numbness or tingling in the limbs
- Difficulty walking or maintaining balance
- Muscle weakness or spasms
- Vision problems, such as blurred or double vision
- Cognitive difficulties, including memory loss or trouble concentrating
- Speech issues, such as slurred speech
- Bowel and bladder dysfunction
These symptoms can appear suddenly or develop gradually over time. They may also come and go, with periods of remission followed by relapses.
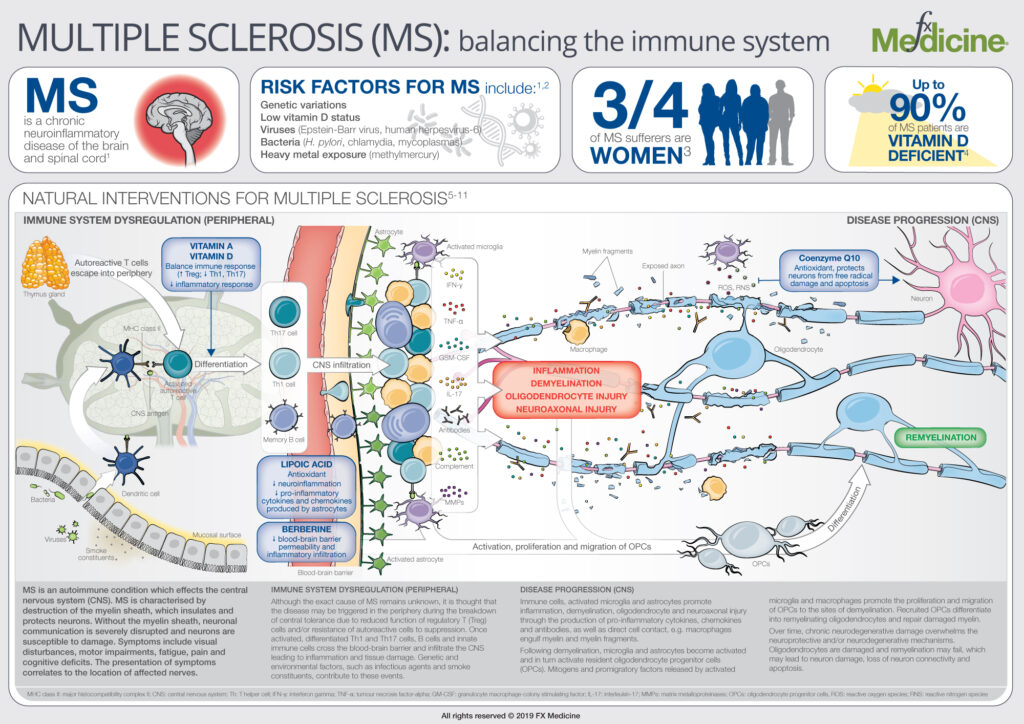
Potential Triggers of Multiple Sclerosis
While the exact cause of this neurological condition remains unknown, researchers have identified several factors that may contribute to its development. These factors include genetic predisposition, environmental influences, and lifestyle choices.
Genetic Factors
Although this condition is not directly inherited, having a family member with the disease increases an individual’s risk. Studies suggest that certain genes may make people more susceptible to developing the condition. However, genetics alone do not determine whether someone will develop it; environmental factors also play a significant role.
Environmental Influences
Several environmental factors have been linked to an increased risk of developing this condition. These include:
- Vitamin D Deficiency: Low levels of vitamin D, often due to insufficient sunlight exposure, have been associated with a higher risk.
- Smoking: Smoking has been shown to increase the likelihood of developing the condition and may also worsen its progression.
- Infections: Certain viral infections, such as the Epstein-Barr virus, have been linked to the onset of the disease.
- Geographical Location: People living farther from the equator, where sunlight exposure is limited, are at a higher risk.
Lifestyle Choices
Unhealthy lifestyle habits, such as poor diet, lack of exercise, and high stress levels, may exacerbate symptoms or contribute to disease progression. Adopting a healthier lifestyle can help manage the condition more effectively.
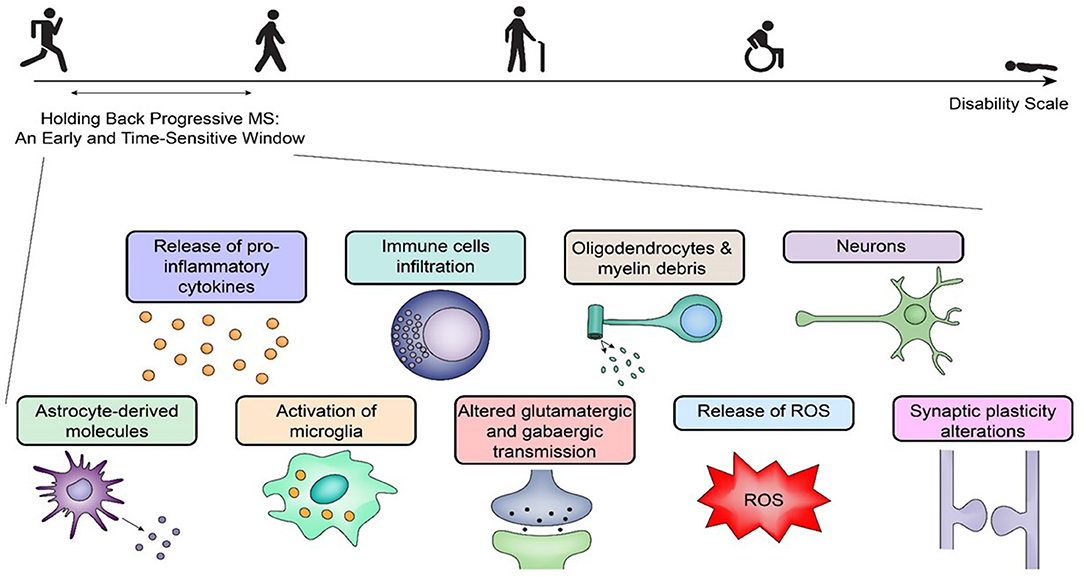
Types of Multiple Sclerosis
This neurological condition manifests in different forms, each with its own pattern of symptoms and progression. Understanding these types can help individuals and healthcare providers tailor treatment plans accordingly.
Relapsing-Remitting Form
This is the most common type, characterized by clearly defined attacks of worsening neurological function, followed by periods of partial or complete recovery. During remission, symptoms may disappear entirely or leave some residual effects.
Primary-Progressive Form
In this type, symptoms worsen steadily over time without distinct periods of relapse or remission. People with this form may experience occasional plateaus or minor improvements, but the overall trend is one of continuous decline.
Secondary-Progressive Form
Many individuals with the relapsing-remitting form eventually transition to this type, where the disease progresses steadily despite occasional flare-ups. The rate of progression varies from person to person.
Progressive-Relapsing Form
This is the rarest type, where the disease progresses steadily from the beginning, with acute relapses occurring along the way. Recovery from these relapses is often incomplete.
Diagnosing Multiple Sclerosis
Diagnosing this condition can be challenging because its symptoms mimic those of other disorders. There is no single test to confirm the diagnosis, so healthcare providers rely on a combination of methods, including:
- Magnetic Resonance Imaging (MRI): This imaging technique helps identify areas of damage in the brain and spinal cord.
- Lumbar Puncture: A sample of cerebrospinal fluid is analyzed for abnormalities, such as elevated levels of certain proteins.
- Evoked Potentials Tests: These tests measure the electrical activity in the brain in response to stimuli, helping detect slowed nerve signal transmission.
A comprehensive evaluation of symptoms, medical history, and test results is essential for an accurate diagnosis.
Treatment and Management Options
While there is currently no cure for this neurological condition, various treatments can help manage symptoms, slow disease progression, and improve quality of life. These treatments fall into three main categories: medications, lifestyle modifications, and alternative therapies.
Medications
Several medications are available to modify the course of the disease and alleviate symptoms:
- Disease-Modifying Therapies: These medications aim to reduce the frequency and severity of relapses while slowing disease progression. Examples include interferons, monoclonal antibodies, and oral medications.
- Symptom Management Drugs: Medications are available to address specific symptoms, such as muscle spasms, fatigue, and bladder dysfunction.
- Steroids: High-dose corticosteroids are often used to reduce inflammation during relapses and speed up recovery.
Lifestyle Modifications
Making healthy lifestyle changes can significantly impact symptom management and overall well-being:
- Exercise: Regular physical activity helps improve strength, flexibility, and mood. Low-impact exercises like swimming and yoga are particularly beneficial.
- Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall health and may reduce inflammation.
- Stress Management: Techniques such as meditation, deep breathing, and mindfulness can help reduce stress, which may trigger symptom flare-ups.
Alternative Therapies
Some individuals find relief through complementary and alternative therapies, though it is important to consult a healthcare provider before trying these options:
- Acupuncture: This traditional Chinese medicine practice involves inserting thin needles into specific points on the body to alleviate pain and improve energy flow.
- Massage Therapy: Massage can help reduce muscle tension, improve circulation, and promote relaxation.
- Herbal Supplements: Certain herbs, such as ginkgo biloba and omega-3 fatty acids, may have anti-inflammatory properties, but their efficacy varies.
Living with Multiple Sclerosis
Living with this condition requires resilience, adaptability, and a proactive approach to health management. Building a strong support network of family, friends, and healthcare professionals is crucial. Additionally, staying informed about the latest research and treatment options empowers individuals to take control of their health journey.
Support groups, both in-person and online, provide valuable opportunities to connect with others facing similar challenges. Sharing experiences and coping strategies can foster a sense of community and reduce feelings of isolation.
Advances in Research
Ongoing research continues to shed light on the underlying mechanisms of this neurological condition and explore innovative treatment approaches. Scientists are investigating the role of gut microbiota, stem cell therapy, and personalized medicine in managing the disease. These advancements offer hope for improved outcomes and, ultimately, a cure.