Migraine is a neurological condition that affects millions of people worldwide. Often abbreviated as “migraine headaches,” these episodes are far more than just a simple headache. They can be debilitating, causing severe pain, nausea, and sensitivity to light and sound. This article delves into the causes, symptoms, and treatments of migraines to provide a comprehensive understanding of this complex condition.
What Is Migraine?
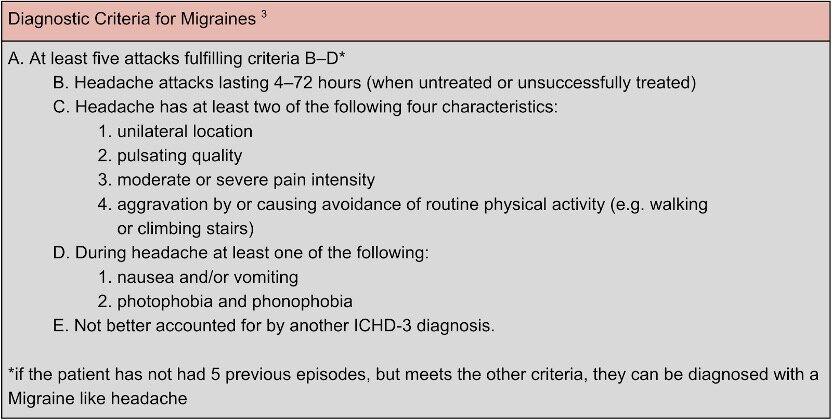
A migraine is a type of headache disorder characterized by recurrent episodes of moderate to severe head pain. These episodes are often accompanied by other symptoms such as nausea, vomiting, and heightened sensitivity to external stimuli like light, sound, or even smells. Unlike tension headaches, which are typically caused by stress or muscle strain, migraines have a more complex origin involving the brain’s chemistry and nervous system.
The duration of a migraine attack can vary widely, lasting anywhere from a few hours to several days. Some individuals experience warning signs before the onset of a migraine, known as an aura, while others do not. The unpredictable nature of migraines makes them particularly challenging for those who suffer from them.
Causes of Migraine
The exact cause of migraines is still not fully understood, but researchers believe they result from a combination of genetic, environmental, and neurological factors. Below are some of the most common contributing factors:
Genetic Predisposition
Migraines often run in families, suggesting a genetic component to the condition. If one or both parents experience migraines, their children are more likely to develop them as well. Studies have identified specific genes that may play a role in migraine susceptibility, although more research is needed to fully understand the genetic mechanisms involved.
Hormonal Changes
Hormonal fluctuations are a significant trigger for many people, especially women. Migraines are often linked to changes in estrogen levels, which occur during menstruation, pregnancy, or menopause. Some women report that their migraines improve during pregnancy, while others find that hormonal contraceptives either alleviate or exacerbate their symptoms.
Environmental Triggers
- Stress: Emotional stress is one of the most common triggers of migraines. The body’s response to stress can lead to chemical changes in the brain that contribute to migraine attacks.
- Dietary Factors: Certain foods and beverages, such as aged cheeses, processed meats, alcohol (especially red wine), and caffeine, can trigger migraines in susceptible individuals.
- Sleep Patterns: Both lack of sleep and excessive sleep can act as triggers. Maintaining a consistent sleep schedule is crucial for managing migraines.
- Weather Changes: Sudden shifts in weather, such as changes in barometric pressure, temperature, or humidity, can provoke migraines in some people.
Neurological Factors
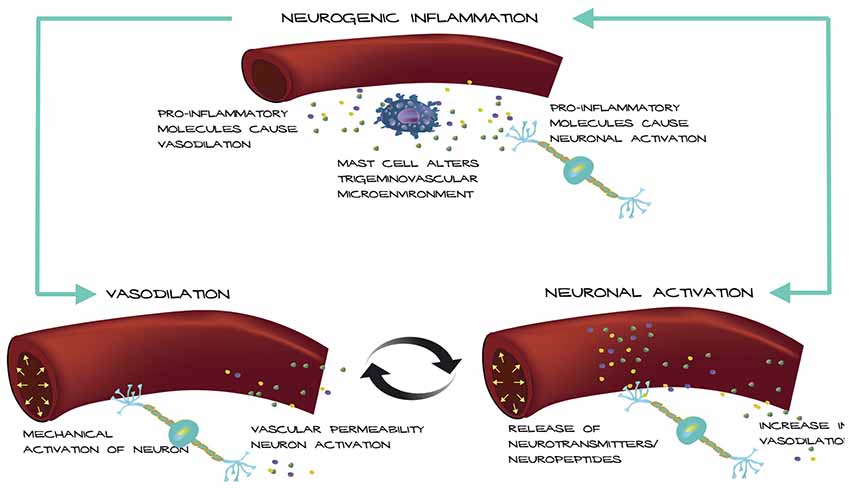
Migraines are believed to involve abnormal brain activity that temporarily affects nerve signals, chemicals, and blood flow in the brain. During a migraine attack, certain areas of the brain become hyperactive, leading to the release of inflammatory substances that irritate nerves and cause pain. This process explains why migraines are classified as a neurological disorder rather than just a headache.
Symptoms of Migraine
Migraines are often divided into four distinct phases, although not everyone experiences all of them. Understanding these phases can help individuals recognize the onset of a migraine and take steps to manage it effectively.
Prodrome Phase
The prodrome phase occurs hours or even days before the actual headache begins. It serves as an early warning sign and may include symptoms such as:
- Mood changes, ranging from depression to euphoria
- Increased thirst and urination
- Frequent yawning
- Food cravings
- Neck stiffness
Aura Phase
Approximately one-third of people with migraines experience an aura, which typically occurs shortly before or during the headache phase. Aura symptoms are usually visual but can also affect other senses. Common manifestations include:
- Flashing lights or zigzag patterns in vision
- Temporary vision loss
- Tingling sensations in the face or hands
- Difficulty speaking or understanding language
While auras can be alarming, they usually last only 20 to 60 minutes and resolve on their own.
Headache Phase
This is the most debilitating phase of a migraine, characterized by intense, throbbing pain that is often localized to one side of the head. Other symptoms during this phase may include:
- Nausea and vomiting
- Sensitivity to light, sound, and smells
- Blurred vision
- Lightheadedness or fainting
The headache phase can last anywhere from four to 72 hours if left untreated.
Postdrome Phase
After the headache subsides, individuals may enter the postdrome phase, sometimes referred to as a “migraine hangover.” During this period, they may feel fatigued, confused, or irritable. Some people report feeling unusually refreshed, while others struggle with lingering cognitive difficulties.
Treatments for Migraine
Managing migraines involves a combination of lifestyle adjustments, preventive measures, and acute treatments. The goal is to reduce the frequency and severity of attacks while alleviating symptoms when they occur.
Lifestyle Modifications
Making certain lifestyle changes can significantly reduce the likelihood of migraines. These include:
- Maintaining a regular sleep schedule
- Eating balanced meals at consistent times
- Staying hydrated throughout the day
- Engaging in regular physical activity
- Practicing stress management techniques, such as meditation or yoga
Acute Treatments
Acute treatments aim to relieve symptoms once a migraine has started. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, may be effective for mild cases. For more severe migraines, prescription medications called triptans are often used. These drugs work by constricting blood vessels and blocking pain pathways in the brain.
In addition to medication, some individuals find relief through non-pharmacological methods, such as applying cold compresses to the head, resting in a dark room, or practicing relaxation techniques.
Preventive Treatments
For individuals who experience frequent or severe migraines, preventive treatments may be necessary. These therapies aim to reduce the frequency and intensity of attacks. Common preventive measures include:
- Daily medications, such as beta-blockers, antidepressants, or anticonvulsants
- Botox injections, which have been approved for chronic migraine prevention
- Cognitive behavioral therapy to address stress and emotional triggers
- Supplements like magnesium, riboflavin, or coenzyme Q10, which have shown promise in reducing migraine frequency
Emerging Therapies
Recent advancements in medical research have led to new treatment options for migraines. One promising development is the use of calcitonin gene-related peptide inhibitors, which target a protein involved in migraine attacks. These medications are administered via injection or infusion and have shown efficacy in reducing the number of monthly migraine days.
Another emerging therapy is neuromodulation devices, which deliver electrical or magnetic stimulation to specific nerves in the brain. These devices offer a non-invasive alternative for individuals who cannot tolerate traditional medications.
Living with Migraine
While there is currently no cure for migraines, understanding the condition and implementing effective management strategies can greatly improve quality of life. Keeping a detailed headache diary can help identify triggers and track the effectiveness of treatments. Working closely with healthcare providers ensures personalized care tailored to individual needs.
Education and advocacy also play vital roles in living with migraines. Raising awareness about the condition helps reduce stigma and fosters empathy among family, friends, and colleagues. Support groups and online communities provide valuable resources and encouragement for those navigating the challenges of migraines.