A meningioma is a type of brain tumor that arises from the meninges, which are the protective membranes covering the brain and spinal cord. Often abbreviated as “MBT” in medical discussions, this condition is one of the most common types of brain tumors diagnosed in adults. Meningiomas are typically slow-growing and benign, but they can sometimes be malignant or cause significant health issues depending on their size and location. In this article, we will explore the key aspects of meningioma brain tumors, including their causes, symptoms, diagnostic methods, and available treatments.
Understanding Meningiomas
Meningiomas originate in the meninges, which consist of three layers: the dura mater, arachnoid mater, and pia mater. These layers protect the central nervous system by cushioning the brain and spinal cord. While meningiomas are most commonly found in the brain, they can also develop along the spinal cord. The majority of meningiomas are noncancerous, meaning they do not spread to other parts of the body. However, even benign meningiomas can cause problems if they grow large enough to press on nearby brain tissue or nerves.
Types of Meningiomas
- Benign Meningiomas: These are the most common type and tend to grow slowly. They rarely invade surrounding tissues.
- Atypical Meningiomas: These tumors grow more aggressively than benign ones and have a higher risk of recurrence after treatment.
- Malignant Meningiomas: Also known as anaplastic meningiomas, these are rare and highly aggressive, with a tendency to invade nearby structures and spread to other areas.
Causes and Risk Factors
The exact cause of meningiomas is not fully understood, but researchers have identified several factors that may increase the risk of developing this condition.
Potential Causes
Meningiomas often result from genetic mutations that occur in the cells of the meninges. These mutations cause the cells to grow and divide uncontrollably, leading to the formation of a tumor. While the precise triggers for these mutations remain unclear, certain factors have been linked to an increased likelihood of developing meningiomas.
Risk Factors
- Age: Meningiomas are more common in adults, particularly those over the age of 60.
- Gender: Women are more likely to develop meningiomas than men, suggesting a possible hormonal connection.
- Radiation Exposure: Previous exposure to high doses of radiation, especially to the head or neck, increases the risk of developing meningiomas.
- Genetic Disorders: Conditions such as neurofibromatosis type 2 are associated with a higher risk of meningiomas.
- Hormonal Factors: Some studies suggest that hormones, particularly estrogen and progesterone, may play a role in the development of meningiomas, as evidenced by their higher prevalence in women.
Symptoms of Meningiomas
The symptoms of meningiomas depend on their size, location, and rate of growth. In many cases, small meningiomas may not cause any noticeable symptoms and are discovered incidentally during imaging tests for unrelated conditions. However, larger or strategically located meningiomas can lead to a variety of neurological symptoms.
Common Symptoms
- Headaches: Persistent or worsening headaches are a frequent symptom of meningiomas.
- Seizures: Some individuals with meningiomas experience seizures, which may vary in severity.
- Vision Problems: Blurred vision, double vision, or loss of peripheral vision can occur if the tumor presses on the optic nerve or related structures.
- Hearing Loss or Ringing in the Ears: Meningiomas near the auditory nerves may affect hearing.
- Weakened Muscles or Numbness: Depending on the tumor’s location, patients may experience weakness, numbness, or tingling in certain parts of the body.
- Cognitive Changes: Memory problems, difficulty concentrating, or personality changes may occur if the tumor affects brain function.
Diagnosing Meningiomas
Diagnosing meningiomas typically involves a combination of clinical evaluation, imaging studies, and sometimes biopsy. Early and accurate diagnosis is crucial for determining the best course of treatment.
Medical History and Physical Examination
Doctors begin by taking a detailed medical history and performing a physical examination. They may ask about symptoms, their duration, and any potential risk factors. A neurological exam is often conducted to assess brain and nerve function, including reflexes, muscle strength, coordination, and sensory perception.
Imaging Tests
Imaging studies are essential for identifying and characterizing meningiomas. The most commonly used techniques include:
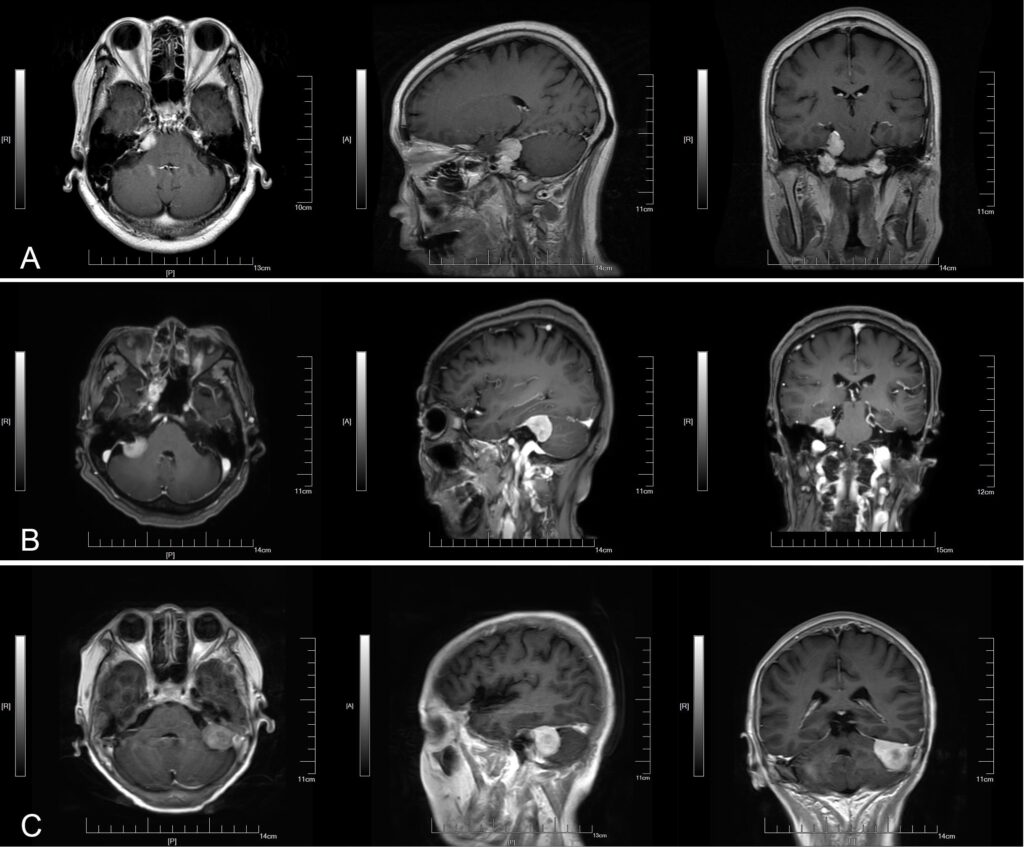
- Magnetic Resonance Imaging: MRI provides detailed images of the brain and spinal cord, helping doctors locate the tumor and assess its size and impact on surrounding structures.
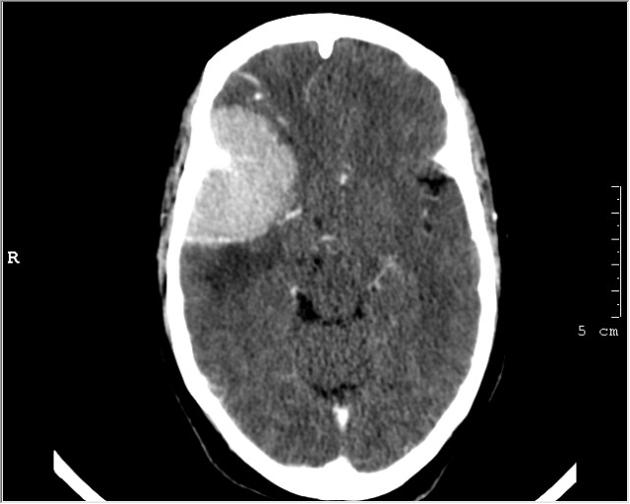
- Computed Tomography Scan: CT scans use X-rays to create cross-sectional images of the brain. They are particularly useful for detecting calcifications within the tumor.
Biopsy
In some cases, a biopsy may be necessary to confirm the diagnosis and determine the tumor’s grade. During a biopsy, a small sample of the tumor is removed and examined under a microscope. This helps differentiate between benign, atypical, and malignant meningiomas.
Treatment Options for Meningiomas
The treatment approach for meningiomas depends on several factors, including the tumor’s size, location, grade, and the patient’s overall health. In some cases, observation may be recommended for small, asymptomatic tumors, while more aggressive treatments are necessary for larger or symptomatic meningiomas.
Observation and Monitoring
For small, slow-growing meningiomas that do not cause symptoms, doctors may recommend regular monitoring through periodic imaging tests. This approach, known as “watchful waiting,” allows healthcare providers to track the tumor’s growth and intervene if necessary.
Surgery
Surgical removal is often the primary treatment for meningiomas, especially if the tumor is causing symptoms or has the potential to grow. The goal of surgery is to remove as much of the tumor as possible without damaging surrounding brain tissue. In some cases, complete removal is achievable, while in others, only partial removal may be possible due to the tumor’s location.
Radiation Therapy
Radiation therapy may be used as a standalone treatment or in combination with surgery. It is particularly beneficial for tumors that cannot be completely removed or for recurrent meningiomas. Types of radiation therapy include:
- External Beam Radiation: High-energy beams are directed at the tumor to destroy cancerous cells.
- Stereotactic Radiosurgery: This precise form of radiation therapy targets the tumor with minimal impact on surrounding tissues.
Medications
While medications are not a primary treatment for meningiomas, they may be prescribed to manage symptoms or side effects. For example, anti-seizure medications can help control seizures, and pain relievers may be used to address headaches.
Emerging Treatments
Researchers are continually exploring new treatment options for meningiomas, including targeted therapies and immunotherapy. These approaches aim to attack specific molecular pathways involved in tumor growth or harness the body’s immune system to fight the tumor.
Living with a Meningioma
Receiving a diagnosis of a meningioma can be overwhelming, but understanding the condition and available treatment options can help patients make informed decisions. Support from healthcare providers, family, and support groups can also play a vital role in managing the emotional and physical challenges associated with this condition.