Marfan Syndrome, often abbreviated as MFS, is a genetic disorder that affects the body’s connective tissue. This condition can impact various systems in the body, including the skeletal, cardiovascular, and ocular systems. While the exact prevalence of Marfan Syndrome varies, it is estimated to affect approximately 1 in 5,000 individuals worldwide. Understanding its causes, recognizing its symptoms, and exploring available treatments are essential for managing this lifelong condition effectively.
What Is Marfan Syndrome?
Marfan Syndrome is a hereditary disorder caused by mutations in the gene responsible for producing fibrillin-1, a protein critical for the formation of elastic fibers in connective tissue. Connective tissue acts as a support system for the body, providing strength and flexibility to structures such as bones, ligaments, blood vessels, and the heart. When this tissue is weakened or malformed due to Marfan Syndrome, it can lead to a wide range of physical and health complications.
The Role of Connective Tissue
Connective tissue serves as the “glue” that holds the body together. It supports organs, provides structure to joints, and ensures the integrity of blood vessels. In individuals with Marfan Syndrome, the defective connective tissue compromises these functions, leading to abnormalities in multiple systems. For example, the weakening of connective tissue in the aorta can result in life-threatening cardiovascular issues, while its impact on the skeleton can cause abnormal growth patterns.
Causes of Marfan Syndrome
Understanding the root cause of Marfan Syndrome is crucial for both prevention and management. The condition is primarily caused by mutations in a specific gene, which can be inherited or occur spontaneously.
Inherited Genetic Mutations
Most cases of Marfan Syndrome are inherited in an autosomal dominant pattern. This means that only one copy of the mutated gene is needed for an individual to develop the condition. If one parent has Marfan Syndrome, there is a 50 percent chance that their child will inherit the disorder. However, not all individuals with the mutated gene exhibit the same severity of symptoms, highlighting the variability of the condition.
Spontaneous Mutations
In approximately 25 percent of cases, Marfan Syndrome occurs due to spontaneous genetic mutations. This means that the mutation arises in the affected individual without being passed down from either parent. Spontaneous mutations can make diagnosing the condition more challenging, as there may be no family history to suggest its presence.
The Role of Fibrillin-1
The gene responsible for Marfan Syndrome is tasked with producing fibrillin-1, a protein that plays a key role in forming microfibrils. Microfibrils are essential components of the extracellular matrix, which provides structural support to tissues. When fibrillin-1 is deficient or abnormal, the resulting connective tissue is weaker and less elastic, leading to the characteristic features of Marfan Syndrome.
Symptoms of Marfan Syndrome
The symptoms of Marfan Syndrome can vary widely, even among members of the same family. Some individuals may experience mild symptoms, while others may face severe complications. These symptoms typically manifest in three primary areas: the skeletal system, the cardiovascular system, and the eyes.
Skeletal Symptoms
One of the most visible signs of Marfan Syndrome is its impact on the skeletal system. Individuals with this condition often exhibit the following characteristics:
- Tall stature with long limbs and fingers
- A narrow and elongated face
- A high-arched palate and crowded teeth
- Scoliosis or an abnormal curvature of the spine
- Pectus excavatum (a sunken chest) or pectus carinatum (a protruding chest)
- Flat feet
These skeletal abnormalities can contribute to joint pain, limited mobility, and an increased risk of fractures.
Cardiovascular Symptoms
The cardiovascular system is particularly vulnerable in individuals with Marfan Syndrome. The most serious complications often involve the heart and blood vessels:
- Dilation of the aorta, which can lead to an aortic aneurysm
- Aortic dissection, a life-threatening condition where the inner layers of the aorta tear
- Mitral valve prolapse, causing the valve between the heart’s chambers to malfunction
- Heart murmurs, which may indicate underlying structural issues
Regular monitoring of cardiovascular health is essential for preventing complications and ensuring timely intervention.
Ocular Symptoms
Marfan Syndrome frequently affects the eyes, leading to a variety of vision-related issues:
- Nearsightedness, which is common among individuals with the condition
- Ectopia lentis, or the displacement of the lens within the eye
- Retinal detachment, a serious condition that requires immediate medical attention
- Glaucoma or cataracts, which may develop at an earlier age than usual
Early detection and treatment of ocular symptoms can help preserve vision and improve quality of life.
Other Symptoms
Beyond the skeletal, cardiovascular, and ocular systems, Marfan Syndrome can also affect other parts of the body. For example:
- Stretch marks on the skin, unrelated to weight changes
- Lung complications, such as spontaneous pneumothorax (collapsed lung)
- Dental issues, including overcrowded teeth and a high-arched palate
These additional symptoms underscore the systemic nature of the condition and highlight the importance of comprehensive care.
Diagnosing Marfan Syndrome
Diagnosing Marfan Syndrome can be challenging due to its variable presentation and overlap with other connective tissue disorders. A thorough evaluation typically involves a combination of clinical assessments, imaging studies, and genetic testing.
Clinical Evaluation
A healthcare provider will begin by conducting a detailed physical examination and reviewing the patient’s medical history. They will look for hallmark features of the condition, such as skeletal abnormalities, cardiovascular irregularities, and ocular symptoms. Family history is also a critical component of the diagnostic process, as it can provide valuable clues about inheritance patterns.
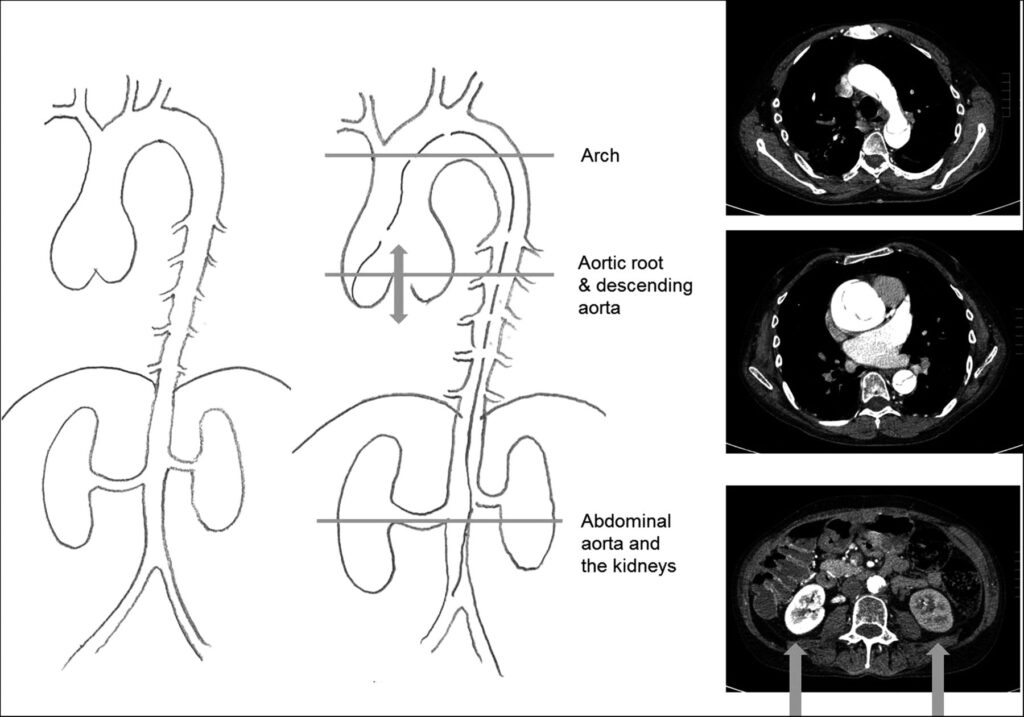
Imaging Studies
Imaging tests play a crucial role in assessing the extent of damage to the cardiovascular system. Echocardiograms are commonly used to evaluate the size and function of the heart and aorta. Magnetic resonance imaging or computed tomography scans may also be employed to obtain detailed images of the aorta and other affected structures.
Genetic Testing
Genetic testing can confirm the presence of mutations associated with Marfan Syndrome. This type of testing is especially useful when the diagnosis is uncertain or when there is no clear family history of the condition. Identifying the specific genetic mutation can also inform treatment decisions and help predict the likelihood of passing the disorder to future generations.
Treatment Options for Marfan Syndrome
While there is currently no cure for Marfan Syndrome, a multidisciplinary approach to treatment can significantly improve outcomes and quality of life. Treatment plans are tailored to address the specific needs of each individual and typically involve a combination of medications, surgical interventions, and lifestyle modifications.
Medications
Medications are often prescribed to manage cardiovascular complications and reduce the risk of life-threatening events. Commonly used medications include:
- Beta-blockers, which slow the heart rate and reduce stress on the aorta
- Angiotensin receptor blockers, which help lower blood pressure and prevent aortic dilation
- Anticoagulants, if mitral valve prolapse leads to irregular heart rhythms
It is essential for individuals with Marfan Syndrome to adhere to their prescribed medication regimen and attend regular follow-up appointments with their healthcare provider.
Surgical Interventions
In some cases, surgery may be necessary to address severe complications. Common surgical procedures include:
- Aortic root replacement, to repair a dilated or damaged aorta
- Mitral valve repair or replacement, to correct valve dysfunction
- Corrective surgeries for scoliosis or pectus deformities
- Procedures to address retinal detachment or ectopia lentis
Surgeries are typically performed by specialists with experience in treating Marfan Syndrome, ensuring optimal outcomes.
Lifestyle Modifications
Adopting certain lifestyle changes can help individuals with Marfan Syndrome manage their symptoms and reduce the risk of complications. Recommended modifications include:
- Avoiding high-intensity sports or activities that place excessive strain on the cardiovascular system
- Maintaining a healthy diet and weight to reduce stress on the heart and joints
- Wearing protective eyewear during physical activities to prevent ocular injuries
- Attending regular check-ups with specialists to monitor disease progression
Education and awareness are also vital components of managing Marfan Syndrome, empowering individuals to take an active role in their care.
Living with Marfan Syndrome
Living with Marfan Syndrome requires ongoing vigilance and collaboration with healthcare providers. Early diagnosis, personalized treatment plans, and proactive management can help individuals lead fulfilling lives despite the challenges posed by the condition. By staying informed and connected to a supportive community, those affected by Marfan Syndrome can navigate their journey with resilience and hope.