Malaria, often abbreviated as “MAL,” is a life-threatening disease caused by parasites transmitted to humans through the bites of infected mosquitoes. It remains one of the most significant public health challenges worldwide, particularly in tropical and subtropical regions. This article explores the causes, symptoms, prevention strategies, and treatment options for this widespread disease.
What Causes Malaria?
Malaria is caused by a group of parasitic organisms belonging to the Plasmodium genus. These parasites are microscopic and invade the human body through the bite of an infected female Anopheles mosquito. There are five species of Plasmodium that can infect humans, with two being the most dangerous:
- Plasmodium falciparum: This species is responsible for the majority of malaria-related deaths and is prevalent in sub-Saharan Africa.
- Plasmodium vivax: This species is more common in South America and Asia and can cause recurring episodes of malaria.
- Plasmodium ovale: A less common species that can also lead to relapses.
- Plasmodium malariae: Known for causing a milder form of malaria but capable of persisting in the body for years.
- Plasmodium knowlesi: Primarily found in Southeast Asia and known to infect both humans and animals.
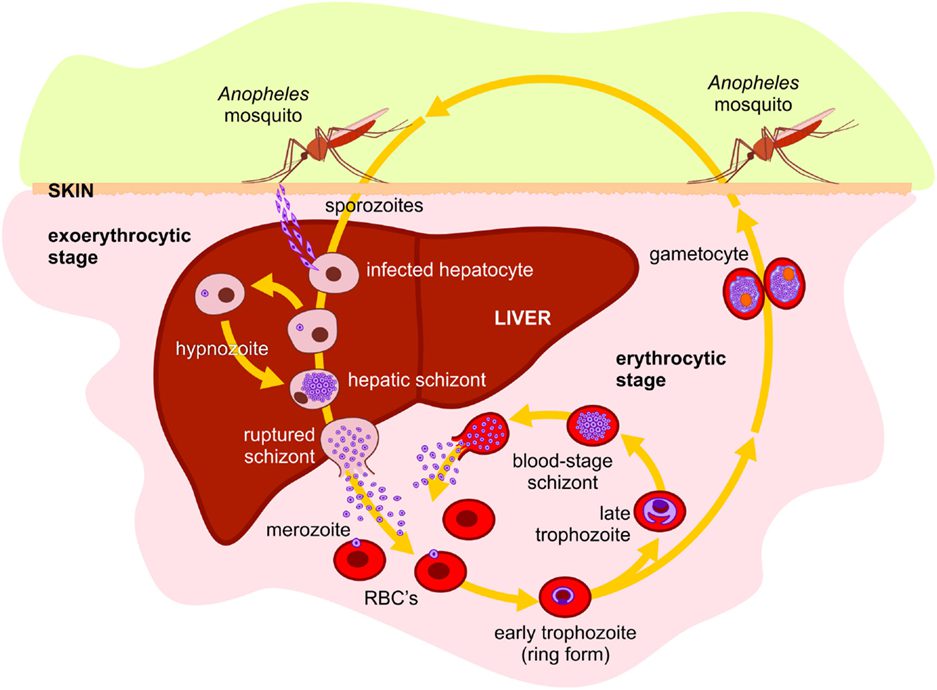
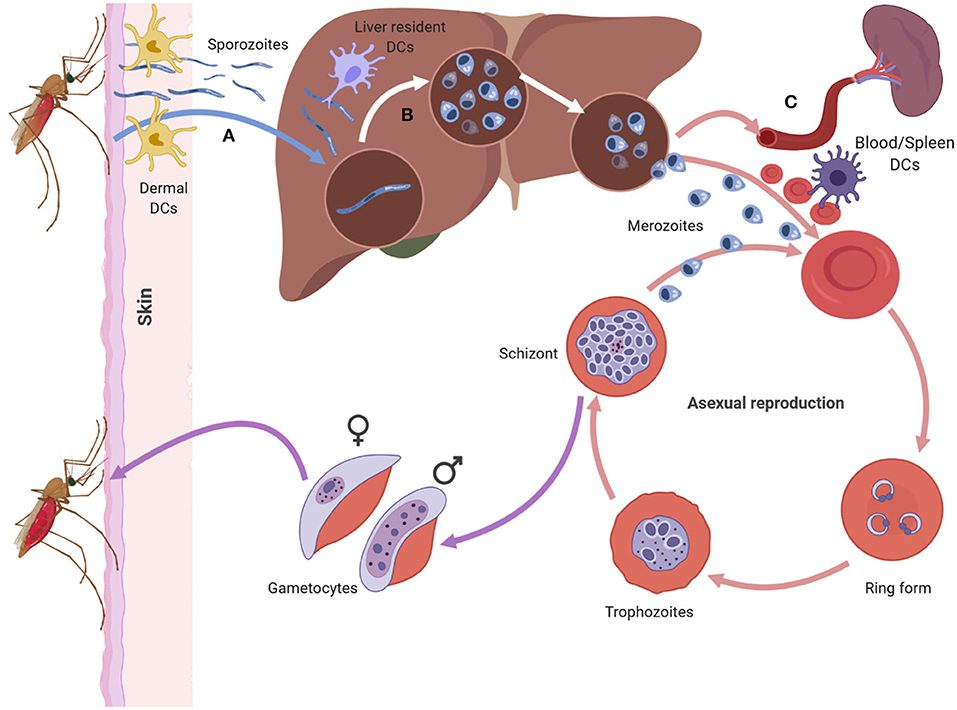
The life cycle of the parasite begins when an infected mosquito bites a human, injecting sporozoites into the bloodstream. These sporozoites travel to the liver, where they mature and multiply. After several days, the parasites re-enter the bloodstream, infecting red blood cells and causing the symptoms of malaria.
Transmission of Malaria
While the primary mode of transmission is through mosquito bites, malaria can also spread through other means:
- Blood transfusions from infected donors.
- Sharing needles or syringes contaminated with infected blood.
- From mother to unborn child during pregnancy (congenital malaria).
It is important to note that malaria cannot be transmitted through casual contact like hugging, kissing, or sharing food.
Symptoms of Malaria
The symptoms of malaria typically appear within ten to fifteen days after being bitten by an infected mosquito. However, in some cases, the onset of symptoms may be delayed due to the type of parasite involved or the use of preventive medications. The most common symptoms include:
- High fever, often accompanied by chills and sweating.
- Severe headaches.
- Muscle pain and fatigue.
- Nausea and vomiting.
- Diarrhea.
- Anemia due to the destruction of red blood cells.
- Jaundice, which is characterized by yellowing of the skin and eyes.
Complications of Severe Malaria
If left untreated, malaria can progress to severe forms, leading to life-threatening complications such as:
- Cerebral malaria, which affects the brain and can cause seizures, coma, or death.
- Severe anemia, resulting from the destruction of red blood cells.
- Acute respiratory distress syndrome, causing difficulty in breathing.
- Kidney failure or liver dysfunction.
- Low blood sugar levels, which can be fatal if not addressed promptly.
Children, pregnant women, and individuals with weakened immune systems are at a higher risk of developing severe malaria.
Prevention of Malaria
Preventing malaria involves a combination of personal protection measures, community-based interventions, and public health strategies. Here are some effective ways to prevent malaria:
Use of Mosquito Nets
Insecticide-treated bed nets are one of the most effective tools for preventing malaria. These nets create a physical barrier between humans and mosquitoes while also killing mosquitoes that come into contact with the insecticide. Sleeping under a treated net every night significantly reduces the risk of infection.
Indoor Residual Spraying
This method involves spraying insecticides on the walls and surfaces inside homes where mosquitoes rest. Indoor residual spraying helps to kill mosquitoes before they have a chance to bite humans, making it a valuable tool in malaria-endemic areas.
Antimalarial Medications
For travelers visiting malaria-prone regions, taking antimalarial medications as a preventive measure is crucial. These drugs work by killing the parasites before they can establish an infection in the body. It is essential to consult a healthcare provider to determine the most appropriate medication based on the destination and individual health conditions.
Environmental Management
Reducing mosquito breeding sites is another key strategy in malaria prevention. Stagnant water, such as puddles, ponds, and open containers, provides ideal environments for mosquitoes to lay their eggs. Communities can reduce the mosquito population by draining standing water and using larvicides to kill mosquito larvae.
Vaccination
A malaria vaccine, known as RTS,S/AS01, has been developed and approved for use in certain regions. While it does not provide complete immunity, the vaccine significantly reduces the risk of severe malaria in children. Ongoing research aims to improve the efficacy and availability of malaria vaccines globally.
Treatment of Malaria
Early diagnosis and prompt treatment are critical to managing malaria effectively and preventing complications. If you suspect you have malaria, seek medical attention immediately. Healthcare providers will perform diagnostic tests, such as blood smears or rapid diagnostic tests, to confirm the presence of the parasite.
Antimalarial Drugs
The choice of treatment depends on the type of malaria parasite, the severity of the infection, and the patient’s age and health status. Commonly used antimalarial drugs include:
- Chloroquine: Effective against Plasmodium vivax and Plasmodium malariae but not against drug-resistant strains of Plasmodium falciparum.
- Artemisinin-based combination therapies: Considered the gold standard for treating uncomplicated Plasmodium falciparum malaria.
- Quinine: Often used for severe malaria cases when other treatments are unavailable.
- Primaquine: Used to treat Plasmodium vivax and Plasmodium ovale infections and to prevent relapses.
Management of Severe Malaria
Severe malaria requires hospitalization and intensive medical care. Treatment may include:
- Intravenous administration of antimalarial drugs.
- Supportive care, such as oxygen therapy and fluid management.
- Blood transfusions to address severe anemia.
- Monitoring and treatment of complications like kidney failure or low blood sugar.
Follow-Up Care
After completing the initial treatment, patients should follow up with their healthcare provider to ensure the infection has been fully eradicated. In cases of Plasmodium vivax or Plasmodium ovale, additional medication may be required to prevent relapses.
Raising Awareness and Education
Education plays a vital role in malaria prevention and control. Communities in endemic areas need access to accurate information about the disease, its transmission, and how to protect themselves. Public health campaigns, school programs, and community workshops can help raise awareness and promote behaviors that reduce the risk of malaria.
Role of Healthcare Providers
Healthcare workers are essential in diagnosing, treating, and educating patients about malaria. They can also advocate for policies that support malaria prevention efforts, such as increased funding for mosquito control programs and improved access to diagnostic tools and medications.
Global Efforts to Combat Malaria
International organizations, governments, and non-governmental organizations are working together to eliminate malaria. Initiatives like the Global Fund to Fight AIDS, Tuberculosis, and Malaria have made significant strides in reducing the burden of the disease. Continued investment in research, infrastructure, and community engagement is necessary to achieve the goal of malaria eradication.