Major Depressive Disorder, often abbreviated as MDD, is a serious mental health condition that affects millions of people worldwide. It is characterized by persistent feelings of sadness, hopelessness, and a lack of interest in daily activities. This guide aims to provide a comprehensive overview of Major Depressive Disorder, including its symptoms, causes, diagnosis, treatment options, and coping strategies.
Understanding Major Depressive Disorder
Major Depressive Disorder is more than just feeling down or experiencing temporary sadness. It is a clinical condition that can significantly impair a person’s ability to function in everyday life. People with this disorder may struggle with work, relationships, and even basic self-care. Understanding the nature of this condition is the first step toward managing it effectively.
Symptoms of Major Depressive Disorder
The symptoms of Major Depressive Disorder can vary from person to person, but there are common signs that healthcare professionals look for when diagnosing the condition. These symptoms must persist for at least two weeks to be considered indicative of the disorder. Below is a list of some of the most common symptoms:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in activities once enjoyed
- Significant changes in appetite, leading to weight loss or gain
- Insomnia or excessive sleeping
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Fatigue or loss of energy nearly every day
- Recurrent thoughts of death or suicide
Causes and Risk Factors
The exact cause of Major Depressive Disorder is not fully understood, but research suggests that it arises from a combination of genetic, biological, environmental, and psychological factors. Some of the most significant risk factors include:
- A family history of depression or other mood disorders
- Experiencing traumatic or stressful events, such as the loss of a loved one or financial difficulties
- Chronic medical conditions, such as diabetes, cancer, or heart disease
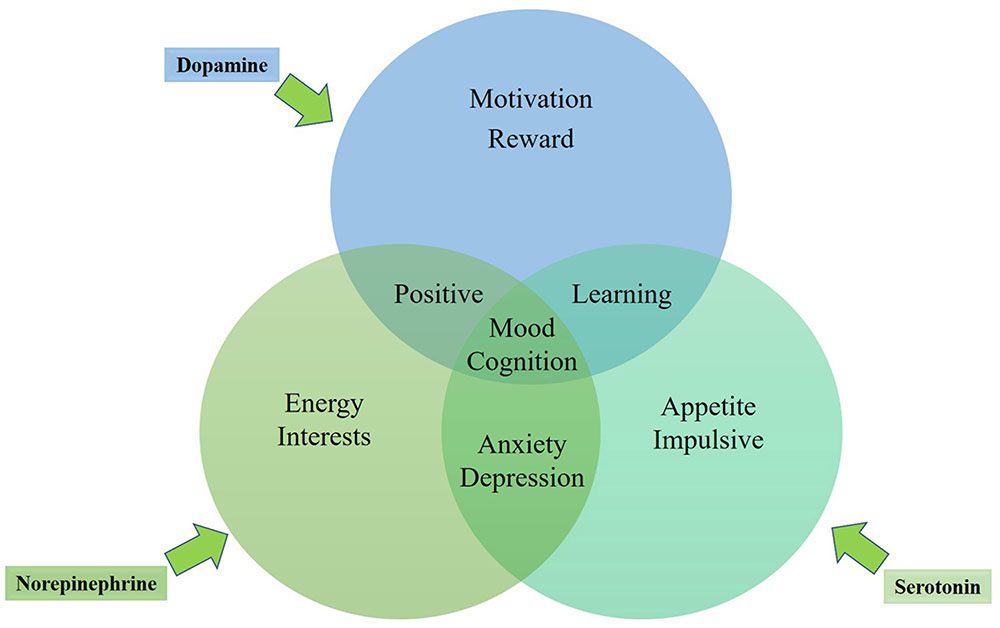
- Imbalances in brain chemicals, such as serotonin and dopamine
- Substance abuse or addiction
- Certain medications that affect mood regulation
Biological Factors
Research has shown that imbalances in neurotransmitters, which are chemicals in the brain responsible for mood regulation, play a significant role in the development of Major Depressive Disorder. Serotonin, dopamine, and norepinephrine are some of the key neurotransmitters involved. Additionally, structural differences in the brains of individuals with depression have been observed, particularly in areas related to emotion regulation and memory.
Environmental Factors
Stressful life events, such as the loss of a job, divorce, or financial instability, can trigger episodes of depression in susceptible individuals. Chronic stress can also lead to changes in the brain that make a person more vulnerable to developing the disorder. Furthermore, a lack of social support or exposure to negative environments during childhood can increase the risk of depression later in life.
Diagnosing Major Depressive Disorder
Diagnosing Major Depressive Disorder involves a thorough evaluation by a healthcare professional, typically a psychiatrist, psychologist, or primary care physician. There is no single test to diagnose the condition, so doctors rely on a combination of methods to reach an accurate conclusion.
Clinical Interviews
One of the primary tools used in diagnosing depression is a clinical interview. During this process, the healthcare provider will ask detailed questions about the patient’s symptoms, medical history, and lifestyle. They may also inquire about any family history of mental health disorders and assess the severity of the symptoms.
Diagnostic Criteria
To meet the criteria for Major Depressive Disorder, a person must experience at least five of the symptoms listed earlier, with one of them being either a depressed mood or a loss of interest in activities. These symptoms must occur nearly every day for at least two weeks and cause significant distress or impairment in daily functioning.
Ruling Out Other Conditions
Because the symptoms of Major Depressive Disorder can overlap with those of other medical and psychiatric conditions, healthcare providers often conduct additional tests to rule out other potential causes. For example, thyroid disorders, vitamin deficiencies, and certain neurological conditions can mimic the symptoms of depression. Blood tests and physical examinations may be performed to ensure an accurate diagnosis.
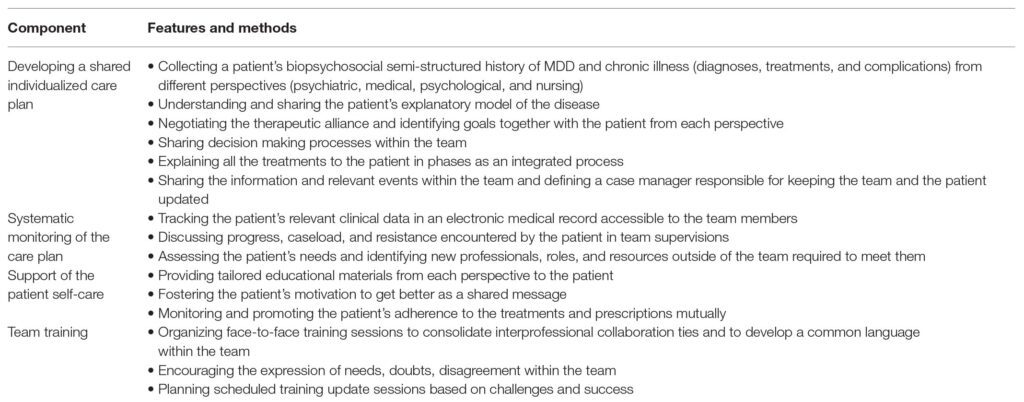
Treatment Options for Major Depressive Disorder
Treatment for Major Depressive Disorder typically involves a combination of psychotherapy, medication, and lifestyle changes. The specific approach depends on the severity of the condition, the individual’s preferences, and their response to previous treatments.
Psychotherapy
Psychotherapy, also known as talk therapy, is one of the most effective treatments for depression. It involves working with a trained therapist to identify and address the underlying causes of the condition. Several types of psychotherapy have been shown to be effective for treating depression:
- Cognitive Behavioral Therapy (CBT): This approach focuses on identifying and changing negative thought patterns and behaviors that contribute to depression.
- Interpersonal Therapy (IPT): IPT helps individuals improve their communication skills and resolve conflicts in relationships that may be contributing to their symptoms.
- Psychodynamic Therapy: This form of therapy explores unconscious processes and past experiences that may be influencing current behavior and emotions.
Medication
Antidepressant medications are commonly prescribed to help manage the symptoms of depression. These medications work by balancing the levels of neurotransmitters in the brain. Some of the most commonly prescribed classes of antidepressants include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): These medications increase the availability of serotonin in the brain and are often the first line of treatment due to their effectiveness and relatively mild side effects.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): These medications target both serotonin and norepinephrine and may be prescribed if SSRIs are not effective.
- Tricyclic Antidepressants (TCAs): Although effective, these older medications are typically reserved for cases where other treatments have failed due to their potential for more severe side effects.
Side Effects of Medication
While antidepressants can be highly effective, they often come with side effects. Common side effects include nausea, weight gain, insomnia, and sexual dysfunction. It is important for individuals to work closely with their healthcare provider to find the right medication and dosage that minimizes side effects while providing relief from symptoms.
Lifestyle Changes
In addition to therapy and medication, making certain lifestyle changes can help alleviate symptoms of depression. These changes may include:
- Engaging in regular physical activity, which has been shown to boost mood and reduce symptoms of depression
- Maintaining a balanced diet rich in nutrients that support brain health, such as omega-3 fatty acids and antioxidants
- Practicing mindfulness techniques, such as meditation or yoga, to reduce stress and improve emotional well-being
- Establishing a consistent sleep routine to improve overall energy levels and cognitive function
Coping Strategies for Living with Depression
Living with Major Depressive Disorder can be challenging, but there are strategies that individuals can use to manage their symptoms and improve their quality of life. These strategies focus on building resilience, fostering supportive relationships, and maintaining a sense of purpose.
Building a Support Network
Having a strong support network is crucial for managing depression. Friends, family members, and support groups can provide emotional support, encouragement, and practical assistance during difficult times. Joining a support group, either in person or online, can also help individuals connect with others who are experiencing similar challenges.
Setting Realistic Goals
Depression can make even simple tasks feel overwhelming. Setting small, achievable goals can help individuals regain a sense of control and accomplishment. Breaking larger tasks into smaller steps and celebrating progress, no matter how minor, can foster a sense of achievement and motivation.
Practicing Self-Compassion
Individuals with depression often struggle with feelings of guilt and self-criticism. Practicing self-compassion involves treating oneself with kindness and understanding, especially during difficult times. This can involve reframing negative thoughts, practicing gratitude, and reminding oneself that recovery is a gradual process.
Seeking Professional Help
It is important for individuals with depression to seek professional help if they are struggling to manage their symptoms on their own. Mental health professionals can provide guidance, support, and evidence-based treatments to help individuals navigate their journey toward recovery.
When to Seek Emergency Help
If someone is experiencing thoughts of self-harm or suicide, it is critical to seek emergency help immediately. These thoughts are a sign of severe depression and should not be ignored. Contacting a crisis hotline, visiting an emergency room, or reaching out to a trusted friend or family member can provide immediate support and intervention.
Major Depressive Disorder is a complex and challenging condition, but with the right treatment and support, individuals can achieve meaningful recovery and lead fulfilling lives.