Lymphedema, often abbreviated as LE, is a chronic condition that arises when the lymphatic system fails to function properly. This leads to an abnormal buildup of fluid in the tissues, causing swelling, discomfort, and potential complications if left untreated. While the abbreviation LE might be convenient, it is essential to delve deeper into what this condition entails, its causes, symptoms, diagnosis, and management options. In this article, we will explore lymphedema comprehensively to provide a better understanding of this complex disorder.
What is the Lymphatic System?
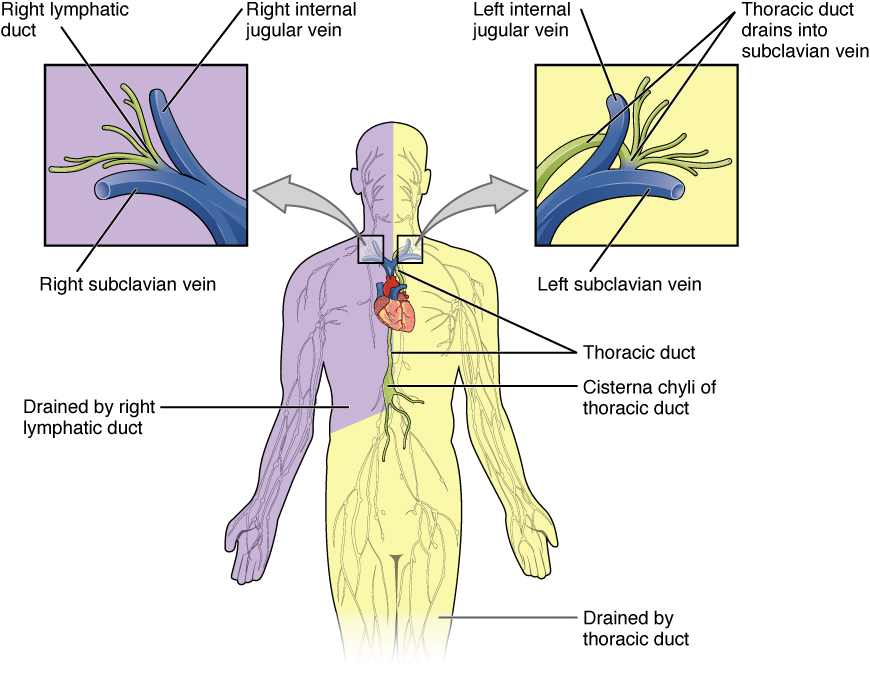
The lymphatic system is a crucial part of the body’s immune and circulatory systems. It consists of a network of vessels, nodes, and organs that work together to maintain fluid balance, filter harmful substances, and support the immune response. The primary role of the lymphatic system is to transport lymph, a clear fluid containing white blood cells, proteins, and waste products, throughout the body. When this system is disrupted or damaged, it can lead to the development of lymphedema.
How Does the Lymphatic System Work?
- Fluid Transport: The lymphatic vessels collect excess fluid from tissues and return it to the bloodstream.
- Filtration: Lymph nodes act as filters, trapping bacteria, viruses, and other harmful particles.
- Immune Support: Lymphocytes, a type of white blood cell, are produced and stored in the lymph nodes to fight infections.
When any part of this intricate system is compromised, it can result in the accumulation of lymphatic fluid in specific areas of the body, leading to swelling.
Types of Lymphedema
There are two main types of lymphedema, each with distinct causes and characteristics.
Primary Lymphedema
Primary lymphedema is a rare condition that occurs due to congenital abnormalities in the lymphatic system. It may be present at birth or develop later in life. There are three subtypes of primary lymphedema:
- Congenital Lymphedema: Present at birth or develops before the age of two.
- Lymphedema Praecox: Develops during puberty or young adulthood, typically before the age of 35.
- Lymphedema Tarda: Occurs after the age of 35 and is the least common form of primary lymphedema.
Secondary Lymphedema
Secondary lymphedema is more common and results from damage or disruption to the lymphatic system caused by external factors. Common causes include:
- Surgical procedures, such as the removal of lymph nodes during cancer treatment.
- Radiation therapy for cancer, which can scar or damage lymphatic vessels.
- Infections, such as filariasis, which is caused by parasitic worms.
- Trauma or injury to the lymphatic system.
- Chronic venous insufficiency, where poor circulation leads to fluid buildup.
Symptoms of Lymphedema
The symptoms of lymphedema can vary depending on the severity and location of the condition. Common signs and symptoms include:
- Swelling in one or more limbs, which may extend to the fingers or toes.
- A feeling of heaviness or tightness in the affected area.
- Restricted range of motion due to swelling.
- Recurring infections in the affected limb.
- Thickening or hardening of the skin, known as fibrosis.
It is important to note that lymphedema typically affects only one side of the body, although bilateral cases can occur. Early detection and treatment are crucial to prevent progression and complications.
Diagnosing Lymphedema
Diagnosing lymphedema involves a combination of clinical evaluation, medical history review, and diagnostic tests. A healthcare provider will assess the patient’s symptoms, examine the affected area, and inquire about any underlying conditions or risk factors.
Diagnostic Tests
- Imaging Studies: Techniques such as magnetic resonance imaging, computed tomography scans, or lymphoscintigraphy may be used to visualize the lymphatic system and identify blockages or abnormalities.
- Bioimpedance Spectroscopy: This non-invasive test measures the amount of fluid in the tissues.
- Doppler Ultrasound: Used to evaluate blood flow and rule out other causes of swelling, such as deep vein thrombosis.
Accurate diagnosis is essential to differentiate lymphedema from other conditions that cause swelling, such as venous insufficiency or heart failure.
Treatment Options for Lymphedema
While there is no cure for lymphedema, various treatments can help manage symptoms, reduce swelling, and improve quality of life. Treatment plans are typically tailored to the individual’s needs and the severity of the condition.
Manual Lymphatic Drainage
Manual lymphatic drainage is a specialized massage technique performed by trained therapists. It involves gentle, rhythmic movements to stimulate the flow of lymphatic fluid and redirect it to healthy lymphatic pathways. This therapy can help reduce swelling and improve overall lymphatic function.
Compression Therapy
Compression therapy involves the use of elastic garments, bandages, or devices to apply pressure to the affected area. This helps prevent fluid buildup, promotes lymphatic drainage, and supports the limb. Compression garments are available in various sizes and levels of compression to suit individual needs.
Exercise and Physical Activity
Regular exercise and physical activity are essential components of lymphedema management. Low-impact activities, such as walking, swimming, or yoga, can improve circulation, enhance lymphatic flow, and strengthen muscles. It is important to consult a healthcare provider or physical therapist to design a safe and effective exercise program.
Skin Care
Maintaining proper skin care is crucial to prevent infections and complications. Individuals with lymphedema should keep their skin clean, moisturized, and protected from cuts, scratches, or insect bites. Prompt treatment of any wounds or infections is necessary to avoid further complications.
Surgical Interventions
In severe cases of lymphedema that do not respond to conservative treatments, surgical interventions may be considered. These procedures aim to remove excess tissue, repair damaged lymphatic vessels, or create new pathways for lymphatic drainage. Surgical options include:
- Liposuction to remove excess fatty tissue.
- Lymphaticovenous anastomosis to connect lymphatic vessels to veins.
- Vascularized lymph node transfer to restore lymphatic function.
Preventing Lymphedema
While not all cases of lymphedema can be prevented, certain measures can reduce the risk of developing the condition or minimize its impact. These include:
- Avoiding injuries, burns, or infections in areas at risk of lymphedema.
- Maintaining a healthy weight to reduce strain on the lymphatic system.
- Elevating the affected limb to promote fluid drainage.
- Using compression garments as recommended by a healthcare provider.
- Following a balanced diet and staying hydrated to support overall health.
Living with Lymphedema
Living with lymphedema requires ongoing management and lifestyle adjustments. Individuals with this condition may face emotional and psychological challenges, such as anxiety, depression, or feelings of self-consciousness. Seeking support from healthcare professionals, support groups, or mental health counselors can be beneficial in coping with these challenges.
Education and awareness are key to empowering individuals with lymphedema to take control of their health. By understanding the condition, adhering to treatment plans, and making informed lifestyle choices, people with lymphedema can lead fulfilling lives despite the challenges posed by this chronic disorder.