Chronic pain is a condition that affects millions of people worldwide, significantly impacting their quality of life. Unlike acute pain, which serves as a warning signal for injury or illness, chronic pain persists long after the initial cause has healed. It can stem from a variety of sources, including injuries, medical conditions, and even psychological factors. The complexity of chronic pain makes it challenging to diagnose and manage effectively. This article delves into the underlying causes, different types, and strategies for managing chronic pain, aiming to provide a comprehensive understanding of this pervasive issue.
What is Chronic Pain?
Chronic pain is defined as pain that lasts for more than three to six months. While acute pain is typically sharp and temporary, chronic pain lingers and often becomes a condition in itself. It can manifest in various forms, such as a dull ache, burning sensation, or sharp stabbing feeling. People living with chronic pain often describe it as relentless and exhausting, affecting not only their physical health but also their emotional and mental well-being.
Unlike acute pain, which resolves as the body heals, chronic pain can persist due to changes in the nervous system. These changes may result in heightened sensitivity to pain signals, making even minor discomfort feel unbearable. Understanding the nature of chronic pain is crucial for developing effective management strategies.
Common Causes of Chronic Pain
Chronic pain can arise from a wide range of causes, and identifying the root cause is essential for proper treatment. Below are some of the most common factors contributing to chronic pain:
Injuries
- Accidents: Injuries sustained from car accidents, falls, or sports-related incidents can lead to chronic pain if they damage nerves, muscles, or bones.
- Surgical Procedures: Some individuals experience lingering pain after surgeries due to nerve damage or scar tissue formation.
Medical Conditions
- Arthritis: Both osteoarthritis and rheumatoid arthritis can cause persistent joint pain and inflammation.
- Fibromyalgia: This condition is characterized by widespread musculoskeletal pain, fatigue, and tenderness in specific areas.
- Neuropathy: Nerve damage caused by diabetes, infections, or other conditions can result in chronic pain.
- Migraines: Recurrent headaches that last for hours or days can become a chronic issue for some individuals.
Psychological Factors
While chronic pain is often linked to physical causes, psychological factors can also play a significant role. Stress, anxiety, and depression can exacerbate pain perception and make it more difficult to manage. Additionally, untreated mental health issues may contribute to the development of chronic pain syndromes.
Types of Chronic Pain
Chronic pain can be categorized into several types based on its origin and characteristics. Understanding these distinctions can help healthcare providers tailor treatment plans to individual needs.
Nociceptive Pain
This type of pain arises from actual or potential tissue damage. It is often described as aching, throbbing, or sharp and is commonly associated with conditions like arthritis, fractures, and sprains. Nociceptive pain occurs when specialized nerve endings called nociceptors detect harmful stimuli and send signals to the brain.
Neuropathic Pain
Neuropathic pain results from damage or dysfunction within the nervous system. It is typically described as burning, tingling, or shooting and may occur without any obvious external cause. Conditions such as diabetic neuropathy, multiple sclerosis, and spinal cord injuries are common sources of neuropathic pain.
Psychogenic Pain
Psychogenic pain refers to pain that is influenced by psychological factors rather than physical injury or disease. While the pain experienced is very real, its origins lie in emotional distress, trauma, or mental health disorders. Treating psychogenic pain often requires addressing underlying psychological issues alongside physical symptoms.
Mixed Pain Syndromes
Some individuals experience a combination of nociceptive and neuropathic pain, leading to what is known as mixed pain syndromes. For example, someone with fibromyalgia may have widespread muscle pain (nociceptive) along with nerve-related symptoms (neuropathic).
Impact of Chronic Pain on Daily Life
Living with chronic pain goes beyond physical discomfort; it permeates every aspect of daily life. Individuals may struggle with simple tasks such as walking, lifting objects, or even getting out of bed. The constant presence of pain can lead to fatigue, sleep disturbances, and reduced mobility, further complicating daily routines.
Emotional and Mental Health Challenges
The emotional toll of chronic pain should not be underestimated. Many people experience feelings of frustration, helplessness, and isolation as they navigate life with persistent discomfort. Over time, these emotions can contribute to the development of anxiety and depression, creating a vicious cycle that worsens both mental health and pain levels.
Work and Social Life
Chronic pain can interfere with one’s ability to perform job duties, leading to decreased productivity or even job loss. Social relationships may also suffer as individuals withdraw from activities they once enjoyed due to fear of worsening their pain or feeling misunderstood by others.
Strategies for Managing Chronic Pain
While there is no universal cure for chronic pain, numerous strategies can help individuals manage their symptoms and improve their quality of life. A multidisciplinary approach that combines medical treatments, lifestyle changes, and psychological support often yields the best results.
Medical Treatments
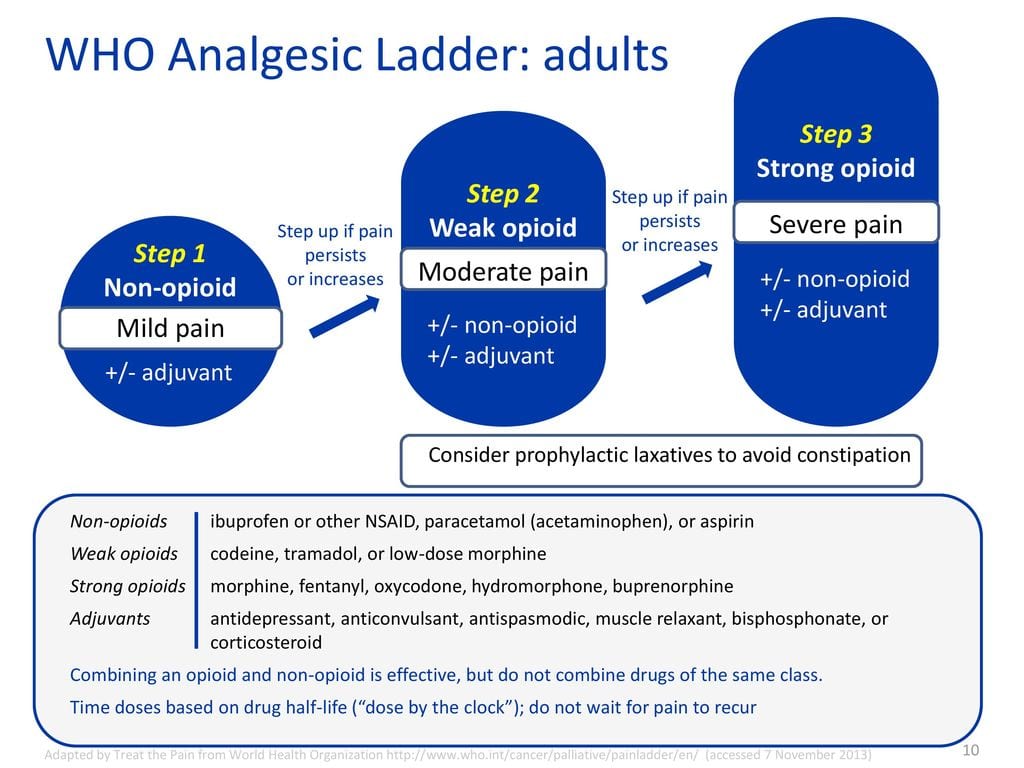
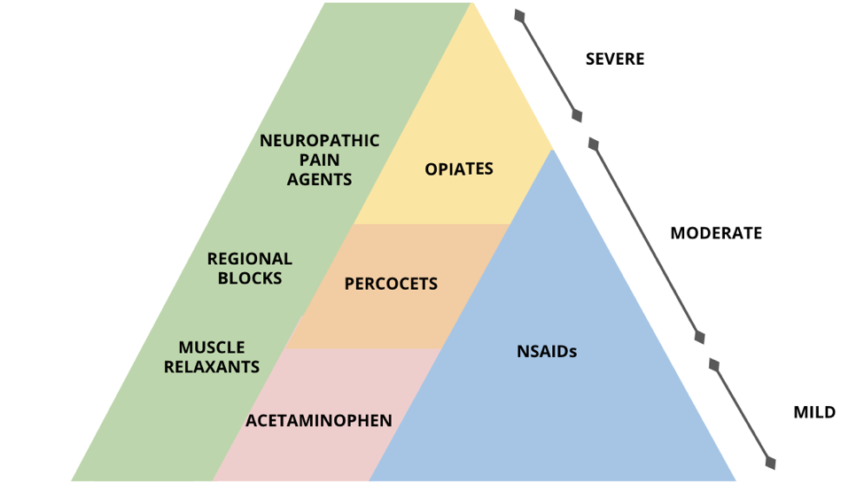
Medications are frequently used to alleviate chronic pain, though they must be carefully prescribed to avoid side effects and dependency risks. Common options include:
- Pain Relievers: Over-the-counter medications like acetaminophen and ibuprofen can provide relief for mild to moderate pain.
- Prescription Medications: Stronger drugs such as opioids, anticonvulsants, and antidepressants may be prescribed for severe cases.
- Injections: Corticosteroid injections can reduce inflammation and relieve localized pain in joints or nerves.
Physical Therapy and Exercise
Physical therapy plays a vital role in managing chronic pain by improving strength, flexibility, and mobility. Tailored exercise programs can help prevent muscle atrophy, enhance circulation, and promote healing. Low-impact activities such as swimming, yoga, and tai chi are particularly beneficial for those with chronic pain.
Alternative Therapies
Many individuals turn to complementary therapies to supplement traditional treatments. Examples include:
- Acupuncture: This ancient practice involves inserting thin needles into specific points on the body to stimulate healing and reduce pain.
- Massage Therapy: Massage can relax tense muscles, improve blood flow, and release endorphins, which are natural painkillers.
- Meditation and Mindfulness: These techniques encourage relaxation and help individuals develop a healthier relationship with their pain.
Lifestyle Modifications
Making certain lifestyle adjustments can significantly impact chronic pain management. Key recommendations include:
- Healthy Diet: Consuming anti-inflammatory foods such as fruits, vegetables, whole grains, and omega-3 fatty acids can support overall health and reduce pain levels.
- Adequate Sleep: Prioritizing good sleep hygiene ensures the body has time to repair itself and cope with stress.
- Stress Management: Engaging in hobbies, practicing deep breathing exercises, or seeking counseling can help mitigate stress-related pain.
Psychological Support
Cognitive-behavioral therapy and other forms of counseling can empower individuals to reframe negative thoughts about their pain and develop coping mechanisms. Group therapy sessions also offer opportunities to connect with others facing similar challenges, fostering a sense of community and understanding.
Emerging Research and Future Directions
As our understanding of chronic pain continues to evolve, researchers are exploring innovative approaches to diagnosis and treatment. Advances in neuroscience, genetics, and technology hold promise for more personalized and effective interventions. For instance, studies on brain imaging techniques aim to identify biomarkers that could predict an individual’s response to specific therapies. Similarly, wearable devices and mobile apps are being developed to monitor pain patterns and deliver real-time feedback to patients and healthcare providers.
Furthermore, ongoing investigations into non-pharmacological treatments, such as virtual reality therapy and biofeedback, highlight the potential for integrating cutting-edge tools into pain management protocols. By embracing a holistic perspective that considers biological, psychological, and social factors, the future of chronic pain care looks increasingly hopeful.