Hepatic Encephalopathy, often abbreviated as HE, is a complex and potentially life-threatening condition that arises due to liver dysfunction. This disorder affects the brain and occurs when the liver is unable to adequately remove toxins from the blood. These toxins, particularly ammonia, accumulate in the bloodstream and travel to the brain, leading to a range of neurological symptoms. Understanding the causes, recognizing the symptoms, and implementing proper care are crucial for managing this condition effectively.
Understanding Liver Brain Disorder
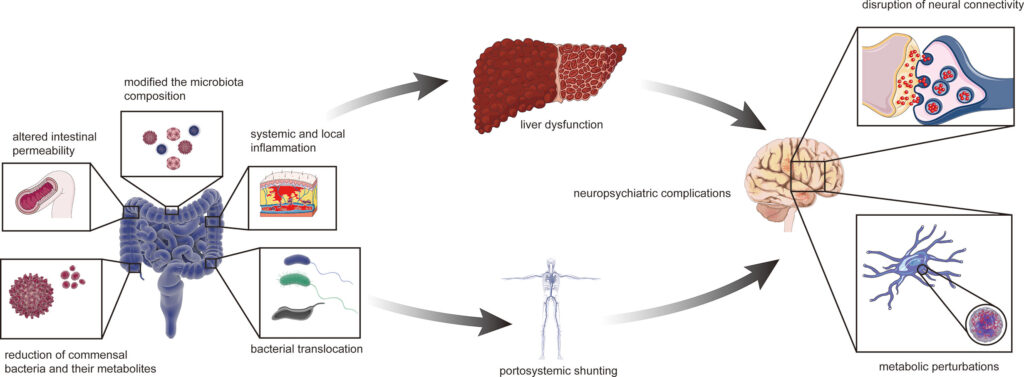
The liver plays a vital role in filtering toxins from the blood. When the liver is damaged or diseased, its ability to perform this function diminishes. As a result, harmful substances such as ammonia can build up in the body and affect brain function. This condition is known as Liver Brain Disorder or Hepatic Encephalopathy. It is most commonly associated with chronic liver diseases like cirrhosis but can also occur in acute liver failure.
How Does the Liver Affect Brain Function?
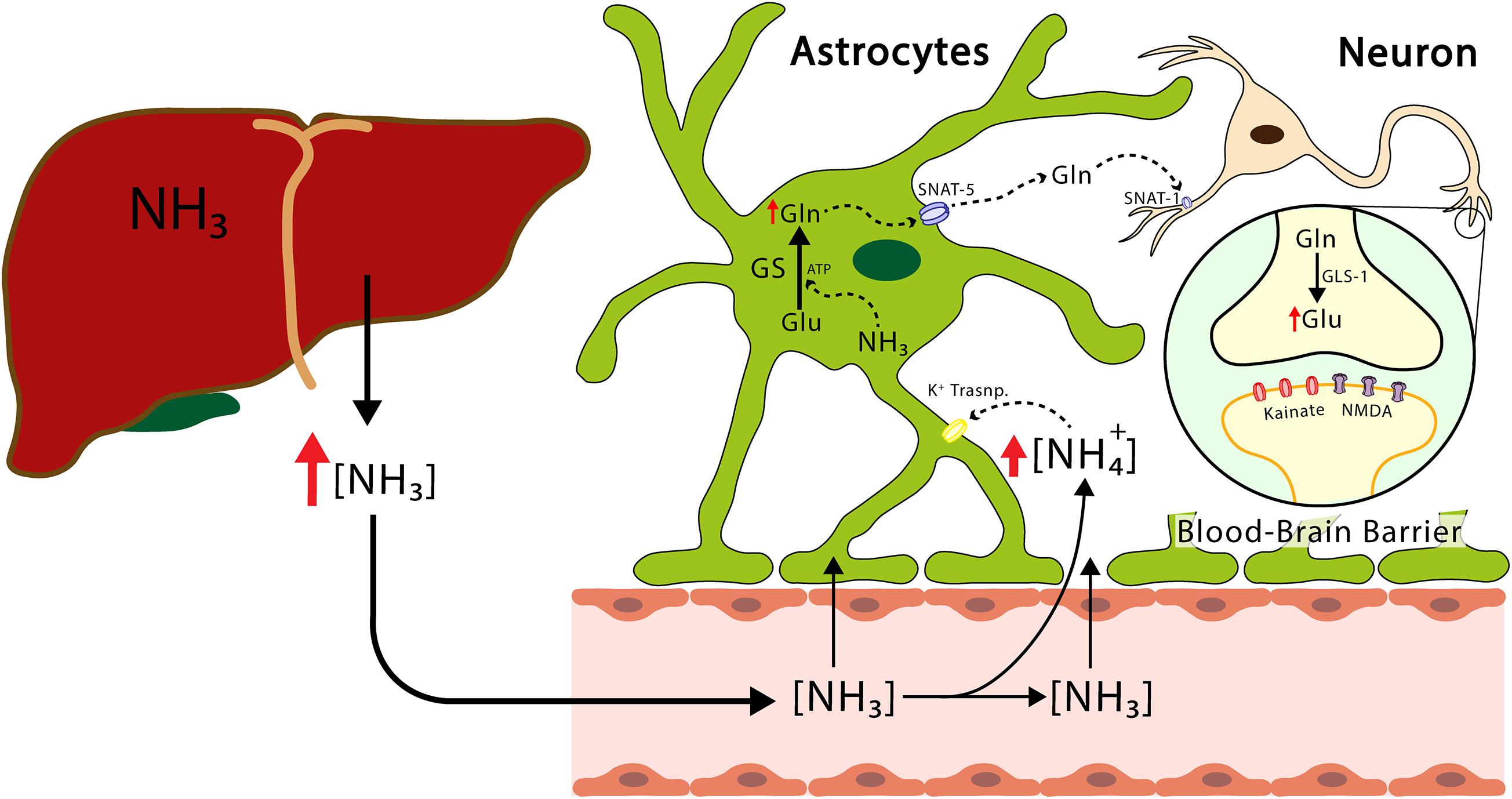
The liver acts as the body’s primary detoxification organ. It processes nutrients, medications, and toxins absorbed from the digestive tract. One of its key functions is converting ammonia, a byproduct of protein metabolism, into urea, which is then excreted through urine. When the liver is compromised, ammonia levels rise in the bloodstream. Elevated ammonia levels interfere with brain function, causing confusion, memory problems, and other neurological issues.
Causes of Liver Brain Disorder
Several factors contribute to the development of this condition. Understanding these causes can help in early detection and prevention.
Chronic Liver Diseases
- Cirrhosis: This is the most common cause of Liver Brain Disorder. Cirrhosis occurs when healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to filter toxins.
- Hepatitis: Chronic viral hepatitis can lead to liver damage over time, increasing the risk of developing this condition.
- Fatty Liver Disease: Both alcoholic and non-alcoholic fatty liver disease can progress to cirrhosis and subsequently increase the risk of brain dysfunction.
Acute Liver Failure
In cases of acute liver failure, the liver suddenly loses its ability to function properly. This can be caused by drug toxicity, viral infections, or autoimmune conditions. The rapid onset of liver dysfunction can quickly lead to elevated toxin levels and brain impairment.
Gastrointestinal Bleeding
Bleeding in the gastrointestinal tract, such as from ulcers or varices, can introduce additional proteins into the bloodstream. The breakdown of these proteins produces more ammonia, overwhelming the already compromised liver and worsening brain function.
Medications and Toxins
Certain medications, such as sedatives and painkillers, can exacerbate Liver Brain Disorder in individuals with pre-existing liver conditions. Additionally, exposure to environmental toxins can further strain the liver and contribute to toxin buildup.
Symptoms of Liver Brain Disorder
The symptoms of this condition vary depending on its severity. They can range from mild cognitive changes to severe neurological impairment. Recognizing these symptoms early is essential for timely intervention.
Mild Symptoms
- Difficulty Concentrating: Individuals may find it hard to focus on tasks or follow conversations.
- Memory Problems: Short-term memory loss or forgetfulness is common in the early stages.
- Mood Changes: Irritability, anxiety, or depression may occur due to the impact of toxins on brain chemistry.
Moderate Symptoms
- Confusion: People may become disoriented about time, place, or person.
- Slurred Speech: Speech may become slow or unclear, resembling intoxication.
- Poor Coordination: Difficulty with fine motor skills, such as writing or buttoning clothes, may develop.
Severe Symptoms
- Extreme Lethargy: Individuals may appear drowsy or unresponsive for extended periods.
- Coma: In advanced cases, the accumulation of toxins can lead to a coma, which is a medical emergency.
Diagnosis of Liver Brain Disorder
Diagnosing this condition involves a combination of clinical evaluation, laboratory tests, and imaging studies. Early diagnosis is critical for preventing complications and improving outcomes.
Clinical Evaluation
Healthcare providers assess the patient’s medical history, symptoms, and physical examination findings. Cognitive tests may be conducted to evaluate memory, attention, and problem-solving abilities.
Laboratory Tests
- Blood Tests: These measure levels of ammonia, liver enzymes, and other markers of liver function.
- Electrolyte Panels: Imbalances in electrolytes can contribute to neurological symptoms.
Imaging Studies
Brain imaging, such as magnetic resonance imaging or computed tomography scans, may be performed to rule out other causes of neurological symptoms, such as strokes or tumors.
Treatment and Management
Managing Liver Brain Disorder requires a comprehensive approach that addresses both the underlying liver disease and the neurological symptoms. Treatment aims to reduce toxin levels, improve liver function, and prevent complications.
Dietary Modifications
A low-protein diet is often recommended to reduce the production of ammonia. However, protein intake should not be eliminated entirely, as it is essential for overall health. Instead, patients are advised to consume plant-based proteins, which are less likely to increase ammonia levels.
Medications
- Lactulose: This medication helps reduce ammonia levels by promoting its excretion through the stool.
- Rifaximin: An antibiotic that decreases the growth of bacteria in the gut, thereby reducing ammonia production.
Treatment of Underlying Liver Disease
Addressing the root cause of liver dysfunction is crucial. For example, antiviral therapy may be prescribed for viral hepatitis, while lifestyle changes are recommended for fatty liver disease. In severe cases, a liver transplant may be necessary.
Management of Triggers
Identifying and avoiding triggers that worsen symptoms is an important aspect of care. Common triggers include dehydration, infections, gastrointestinal bleeding, and certain medications.
Preventive Measures
While Liver Brain Disorder cannot always be prevented, certain measures can reduce the risk of its development or recurrence.
Regular Monitoring
Individuals with chronic liver diseases should undergo regular check-ups to monitor liver function and detect early signs of complications.
Vaccinations
Vaccines for hepatitis A and B can protect against viral infections that may lead to liver damage.
Healthy Lifestyle Choices
- Avoid Alcohol: Alcohol consumption can accelerate liver damage and increase the risk of this condition.
- Balanced Diet: Eating a nutritious diet supports liver health and reduces the risk of fatty liver disease.
- Exercise Regularly: Physical activity helps maintain a healthy weight and reduces the risk of metabolic disorders.
Support for Caregivers and Patients
Caring for someone with Liver Brain Disorder can be challenging, both physically and emotionally. Support from healthcare professionals, family members, and support groups can make a significant difference.
Education and Awareness
Patients and caregivers should be educated about the condition, its symptoms, and treatment options. Understanding the importance of adherence to dietary and medication regimens is crucial for effective management.
Emotional Support
Living with a chronic illness can take a toll on mental health. Counseling, therapy, and support groups provide a safe space to share experiences and coping strategies.
Practical Assistance
Assistance with daily activities, transportation to medical appointments, and meal preparation can alleviate some of the burdens faced by patients and caregivers.
Emerging Research and Innovations
Ongoing research is exploring new treatments and technologies to improve outcomes for individuals with Liver Brain Disorder. Advances in liver transplantation, gene therapy, and artificial liver devices hold promise for the future.
Artificial Liver Devices
These devices aim to temporarily support liver function in patients awaiting transplantation. They work by filtering toxins from the blood, similar to how a healthy liver would.
Gene Therapy
Gene therapy seeks to repair or replace defective genes responsible for liver diseases, potentially offering a long-term solution for patients.
Personalized Medicine
Tailoring treatment plans based on an individual’s genetic makeup and specific liver condition may enhance the effectiveness of therapies and reduce side effects.