Lewy Body Dementia, often abbreviated as LBD, is a progressive brain disorder that affects thinking, movement, behavior, and mood. It is one of the most common types of dementia, following Alzheimer’s disease and vascular dementia. This condition is characterized by the presence of abnormal protein deposits in the brain, known as Lewy bodies, which disrupt normal brain functioning. In this article, we will explore the key aspects of this complex condition, including its symptoms, diagnosis, and care strategies.
What is Lewy Body Dementia?
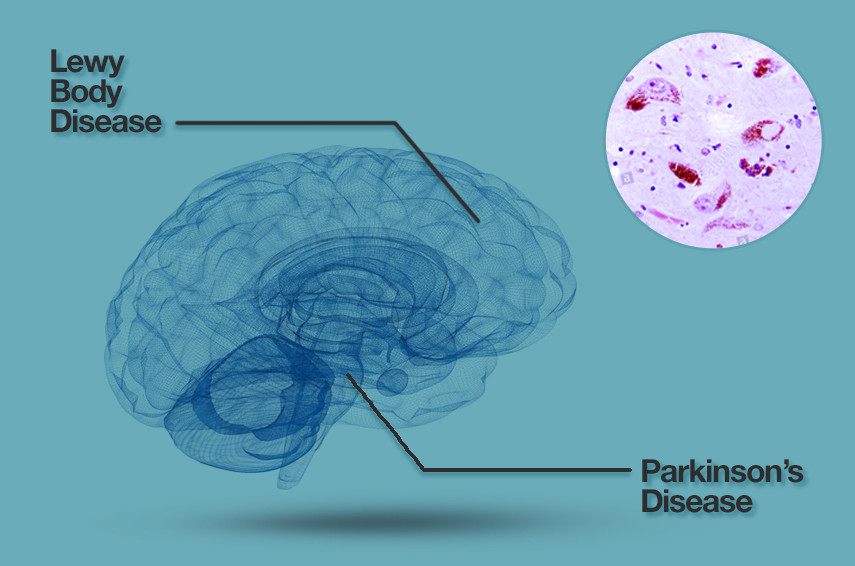
Lewy Body Dementia is a neurodegenerative disorder that leads to a decline in mental abilities, motor skills, and emotional regulation. The disease is named after the abnormal protein deposits found in the brains of affected individuals. These deposits are made up of a protein called alpha-synuclein, which accumulates in nerve cells and interferes with their ability to communicate effectively. As a result, people with this condition experience a wide range of symptoms that can vary significantly from person to person.
This type of dementia is closely related to Parkinson’s disease dementia, as both conditions involve the presence of Lewy bodies. However, they differ in terms of when cognitive symptoms appear relative to motor symptoms. In Lewy Body Dementia, cognitive decline typically occurs early in the disease process, while in Parkinson’s disease dementia, cognitive issues tend to develop later.
Prevalence and Risk Factors
- Prevalence: It is estimated that this form of dementia affects approximately 1.4 million people in the United States alone. Despite its prevalence, it remains underdiagnosed due to its overlapping symptoms with other neurological disorders.
- Risk Factors: Age is the most significant risk factor, with most cases occurring in individuals over the age of 50. Other potential risk factors include a family history of dementia or Parkinson’s disease, as well as certain genetic mutations.
Symptoms of Lewy Body Dementia
The symptoms of this condition can be broadly categorized into cognitive, motor, and psychiatric symptoms. These symptoms often fluctuate in severity, making the condition challenging to diagnose and manage.
Cognitive Symptoms
Cognitive symptoms are among the earliest signs of this condition. They include:
- Memory Loss: While memory problems are less pronounced compared to Alzheimer’s disease, individuals may still struggle with short-term memory and recall.
- Attention and Alertness Fluctuations: People with this condition may experience significant variations in their levels of alertness and attention throughout the day.
- Executive Function Impairment: Difficulties with planning, problem-solving, and multitasking are common.
- Visual-Spatial Challenges: Problems with perceiving spatial relationships and navigating familiar environments can occur.
Motor Symptoms
Movement-related symptoms resemble those seen in Parkinson’s disease. These include:
- Tremors: Shaking, particularly in the hands, is a hallmark symptom.
- Muscle Stiffness: Rigidity in muscles can lead to discomfort and limited mobility.
- Slowed Movements: Known as bradykinesia, this symptom makes everyday tasks more difficult to perform.
- Balanace Issues: Individuals may experience frequent falls due to poor balance and coordination.
Psychiatric Symptoms
In addition to cognitive and motor symptoms, this condition often involves psychiatric manifestations, such as:
- Hallucinations: Visual hallucinations are particularly common and may involve seeing people, animals, or objects that are not there.
- Delusions: False beliefs, such as paranoia or suspicion, can develop.
- Mood Changes: Depression, anxiety, and apathy are frequently reported.
- Sleep Disturbances: REM sleep behavior disorder, where individuals act out their dreams, is a notable feature.
Diagnosis of Lewy Body Dementia
Diagnosing this condition can be challenging due to its overlap with other neurological disorders. A comprehensive evaluation is required to rule out other potential causes of the symptoms.
Medical History and Physical Examination
The diagnostic process begins with a detailed medical history and physical examination. Healthcare providers will inquire about the onset and progression of symptoms, as well as any family history of neurological disorders. During the physical exam, motor symptoms such as tremors and muscle stiffness are assessed.
Cognitive Testing
Cognitive assessments are conducted to evaluate memory, attention, language, and problem-solving abilities. These tests help identify patterns of cognitive decline that are characteristic of this condition.
Imaging Studies
Brain imaging techniques, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), are used to detect structural and functional changes in the brain. While these scans cannot definitively diagnose this condition, they can help rule out other causes of dementia, such as strokes or tumors.
Additional Diagnostic Tools
In some cases, additional tests may be necessary to confirm the diagnosis. These include:
- Sleep Studies: Polysomnography can detect REM sleep behavior disorder, which is strongly associated with this condition.
- Biomarker Research: Emerging research is exploring the use of biomarkers, such as alpha-synuclein levels, to improve diagnostic accuracy.
Care and Management Strategies
While there is currently no cure for this condition, various treatment approaches can help manage symptoms and improve quality of life for both patients and caregivers.
Medications
Several medications are available to address specific symptoms:
- Cholinesterase Inhibitors: These drugs, commonly used in Alzheimer’s disease, can help improve cognitive function and reduce hallucinations.
- Parkinson’s Disease Medications: Levodopa and other medications may alleviate motor symptoms, though they can sometimes worsen psychiatric symptoms.
- Antipsychotics: Certain antipsychotic medications may be prescribed cautiously to manage hallucinations and delusions.
Non-Pharmacological Interventions
In addition to medications, non-drug approaches play a crucial role in managing this condition:
- Physical Therapy: Exercises designed to improve strength, flexibility, and balance can help mitigate motor symptoms.
- Occupational Therapy: This therapy focuses on enhancing daily living skills and promoting independence.
- Cognitive Stimulation: Activities such as puzzles, games, and social interactions can support cognitive health.
Support for Caregivers
Caring for someone with this condition can be emotionally and physically demanding. Support for caregivers is essential and may include:
- Education: Learning about the disease helps caregivers better understand and anticipate challenges.
- Respite Care: Temporary caregiving services provide much-needed breaks for primary caregivers.
- Support Groups: Connecting with others in similar situations offers emotional support and practical advice.
Lifestyle Modifications
Making lifestyle changes can also contribute to better management of symptoms:
- Diet and Nutrition: A balanced diet rich in fruits, vegetables, and omega-3 fatty acids supports brain health.
- Regular Exercise: Physical activity promotes overall well-being and may slow disease progression.
- Sleep Hygiene: Establishing a consistent sleep routine can help manage sleep disturbances.
Research and Future Directions
Ongoing research is focused on understanding the underlying mechanisms of this condition and developing more effective treatments. Scientists are investigating the role of genetics, environmental factors, and immune system responses in disease development. Additionally, clinical trials are exploring new medications and therapies aimed at slowing disease progression and improving symptom management.
Advancements in imaging technology and biomarker research hold promise for earlier and more accurate diagnoses. Increased awareness and education about this condition are also critical to ensuring timely diagnosis and appropriate care.





