Leprosy, also known as Hansen’s Disease, is a chronic infectious disease that primarily affects the skin, peripheral nerves, mucosal surfaces of the upper respiratory tract, and the eyes. Despite being one of the oldest diseases recorded in human history, it continues to be a public health concern in certain parts of the world. Referred to as HD in medical literature, this condition has been surrounded by stigma and misunderstanding for centuries. In this article, we will explore the causes, symptoms, diagnostic methods, and treatment options available for this complex disease.
Understanding the Causes of Leprosy
The primary cause of leprosy is a slow-growing bacterium called Mycobacterium leprae. This microorganism was first identified in 1873 by Gerhard Armauer Hansen, a Norwegian physician, which is why the disease is also named after him. The bacteria thrive in cooler temperatures, which explains why they predominantly infect the skin, peripheral nerves, and other cooler regions of the body.
Transmission of the Disease
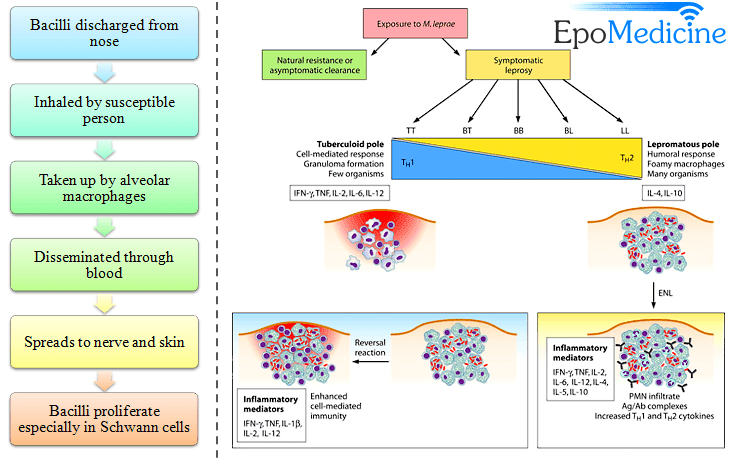
Leprosy spreads through droplets from the nose and mouth of an infected individual during close and prolonged contact. It is important to note that leprosy is not highly contagious, and most people have natural immunity against the bacteria. However, individuals with compromised immune systems or those living in overcrowded and unsanitary conditions are at a higher risk of contracting the disease.
Risk Factors
- Prolonged exposure to untreated cases of leprosy
- Living in regions with poor sanitation and limited access to healthcare
- Genetic predisposition or weakened immune system
- Close contact with armadillos, which can carry the bacteria in some regions
Symptoms of Leprosy
The symptoms of leprosy vary depending on the type and severity of the infection. The disease progresses slowly, and it may take several years for symptoms to appear after initial exposure to the bacteria. Early diagnosis is crucial to prevent complications such as nerve damage and deformities.
Common Signs and Symptoms
- Discolored patches of skin that may feel numb or lack sensation
- Thickened or enlarged peripheral nerves, particularly in the arms and legs
- Muscle weakness or paralysis, especially in the hands and feet
- Ulcers on the soles of the feet due to loss of sensation
- Eye damage leading to blindness if left untreated
- Nasal congestion or nosebleeds caused by damage to the mucous membranes
Types of Leprosy
Leprosy is classified into two main types based on the immune response of the host:
- Tuberculoid Leprosy: This form is characterized by fewer lesions and mild symptoms. The immune system responds strongly to the bacteria, limiting their spread.
- Lepromatous Leprosy: In this more severe form, the immune response is weak, allowing the bacteria to multiply extensively and cause widespread damage to the skin, nerves, and other organs.
A third category, Borderline Leprosy, exhibits characteristics between the two extremes and can shift toward either tuberculoid or lepromatous forms depending on the immune response.
Diagnosis of Leprosy
Early and accurate diagnosis is essential to prevent complications and reduce the transmission of leprosy. Since the symptoms can mimic other skin conditions, healthcare providers rely on a combination of clinical evaluation, laboratory tests, and imaging studies to confirm the presence of the disease.
Clinical Examination
A healthcare professional will examine the patient’s skin for discolored patches, nodules, or thickened nerves. They may also assess sensory loss by testing the ability to feel touch, pain, or temperature in affected areas.
Laboratory Tests
Several laboratory techniques are used to detect Mycobacterium leprae:
- Skin Smear Test: A small sample of skin or fluid from a lesion is examined under a microscope to identify the bacteria.
- Histopathological Examination: A biopsy of the affected tissue is analyzed to detect characteristic changes caused by the bacteria.
- Polymerase Chain Reaction (PCR): This advanced molecular test amplifies bacterial DNA to confirm the presence of Mycobacterium leprae.
Imaging Studies
In cases where nerve involvement is suspected, imaging techniques such as ultrasound or magnetic resonance imaging may be used to evaluate the extent of nerve damage.
Treatment Options for Leprosy
Leprosy is curable with multidrug therapy, which involves the use of multiple antibiotics to eliminate the bacteria and prevent drug resistance. The World Health Organization provides free treatment for all diagnosed cases, making it accessible even in low-income regions.
Medications Used in Treatment
The specific drugs and duration of treatment depend on the type and severity of leprosy. Commonly prescribed medications include:
- Dapsone: An antibiotic that inhibits the growth of Mycobacterium leprae.
- Rifampicin: A powerful antibiotic that kills the bacteria directly.
- Clofazimine: An antimicrobial agent that also reduces inflammation and prevents relapse.
For tuberculoid leprosy, treatment typically lasts six months, while lepromatous leprosy requires a longer course of up to twelve months. Patients must adhere strictly to the prescribed regimen to ensure complete recovery and minimize the risk of relapse.
Management of Complications
In addition to antibiotics, patients may require supportive care to address complications such as nerve damage, deformities, and secondary infections. Physical therapy and occupational therapy can help restore mobility and improve quality of life. In severe cases, reconstructive surgery may be necessary to correct deformities or restore function.
Prevention of Disability
Early detection and treatment play a critical role in preventing disability caused by leprosy. Patients are educated on self-care practices, such as inspecting their hands and feet daily for injuries, wearing protective footwear, and avoiding activities that strain affected nerves. Regular follow-up visits with healthcare providers ensure timely intervention if complications arise.
Addressing Stigma and Social Challenges
Despite advances in medical science, leprosy remains shrouded in stigma and discrimination. Many affected individuals face social isolation, loss of employment, and psychological distress due to misconceptions about the disease. Community awareness programs and advocacy efforts are vital to dispel myths and promote inclusivity.
Role of Education and Awareness
Educating communities about the causes, transmission, and treatment of leprosy can reduce fear and prejudice. Schools, healthcare facilities, and religious organizations can collaborate to spread accurate information and encourage empathy toward those affected by the disease.
Support for Affected Individuals
Non-governmental organizations and support groups provide counseling, vocational training, and financial assistance to help individuals reintegrate into society. These initiatives empower patients to lead fulfilling lives and contribute positively to their communities.
Ongoing Research and Future Directions
While significant progress has been made in combating leprosy, challenges remain in eliminating the disease globally. Researchers are exploring new diagnostic tools, vaccines, and therapeutic strategies to enhance prevention and treatment outcomes.
Vaccine Development
The Bacillus Calmette-Guérin vaccine, commonly used to prevent tuberculosis, offers partial protection against leprosy. Scientists are working on developing a more effective vaccine specifically targeting Mycobacterium leprae.
Advances in Diagnostics
Innovations in rapid diagnostic tests and point-of-care devices aim to facilitate early detection, especially in remote areas with limited access to healthcare facilities.
Global Efforts Toward Eradication
International partnerships between governments, non-profit organizations, and research institutions are strengthening surveillance systems and improving access to treatment. These collaborative efforts are paving the way toward a world free of leprosy.





