Leg pain while walking, often referred to as claudication, is a common condition that affects many individuals, particularly those over the age of fifty. The term “claudication” originates from the Latin word for “limping,” which aptly describes the primary symptom experienced by sufferers. This type of discomfort typically arises during physical activity and subsides with rest. Understanding the underlying causes, recognizing the symptoms, and exploring treatment options can significantly improve quality of life for those affected.
What Is Leg Pain While Walking?
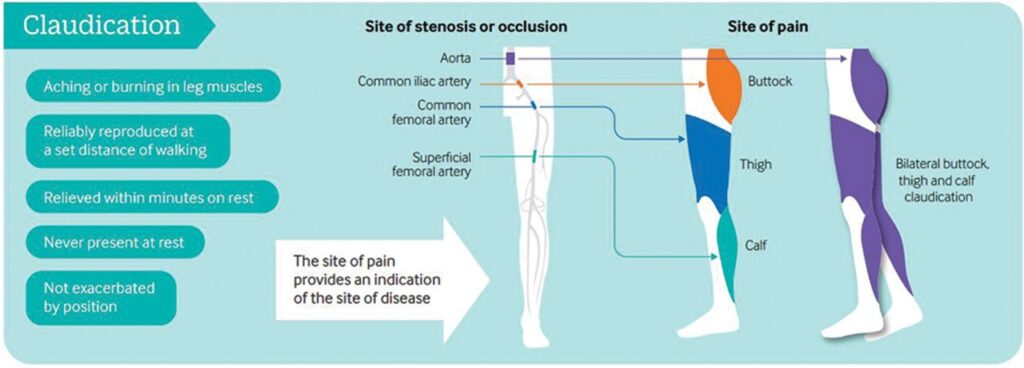
Leg pain while walking occurs when there is insufficient blood flow to the muscles in the legs during physical exertion. This lack of blood flow leads to oxygen deprivation, causing cramping, aching, or fatigue in the muscles. The pain usually begins after walking a certain distance or climbing stairs and tends to disappear after a short period of rest. Although it may seem like a minor inconvenience, this condition can indicate more serious underlying health issues if left untreated.
How Does It Differ From Other Types of Leg Pain?
Unlike general muscle soreness or joint pain, leg pain while walking is specifically linked to reduced circulation. Muscle soreness from exercise tends to occur immediately after the activity and improves with movement, whereas this condition worsens with continued walking and only improves with rest. Joint-related pain, such as arthritis, typically persists regardless of activity levels and does not follow the same pattern of onset and relief.
Common Causes of Leg Pain While Walking
Several factors contribute to the development of leg pain while walking. Identifying the root cause is essential for effective management and treatment.
Peripheral Artery Disease
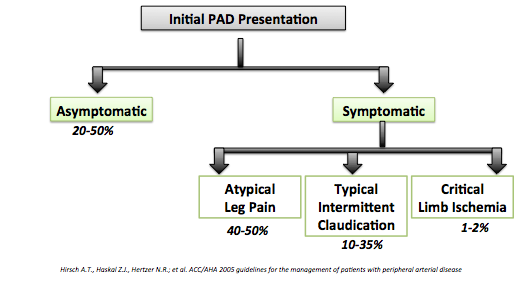
One of the most common causes of leg pain while walking is peripheral artery disease. This condition occurs when fatty deposits, known as plaques, build up inside the arteries, narrowing them and restricting blood flow. As a result, the muscles in the legs do not receive enough oxygen-rich blood during physical activity, leading to pain and discomfort.
Blood Clots
Blood clots can also obstruct blood flow to the legs, causing pain during movement. These clots may form due to prolonged immobility, injury, or underlying medical conditions such as deep vein thrombosis. If a clot breaks loose and travels to other parts of the body, it can pose a life-threatening risk, making early detection critical.
Spinal Stenosis
Spinal stenosis refers to the narrowing of the spinal canal, which places pressure on the nerves traveling through the lower back and into the legs. This compression can lead to pain, numbness, or weakness in the legs, especially during activities like walking. Unlike circulatory issues, spinal stenosis-related pain may be relieved by leaning forward or sitting down.
Muscle Strain or Injury
In some cases, leg pain while walking may stem from muscle strain or injury rather than circulatory problems. Overuse, poor conditioning, or sudden increases in physical activity can all contribute to muscle-related discomfort. While this type of pain is generally less serious, it can still interfere with daily activities and should not be ignored.
Symptoms to Watch For
Recognizing the symptoms of leg pain while walking is crucial for seeking timely medical attention. The following signs are commonly associated with this condition:
- Cramping or Aching: A deep, aching sensation in the calf, thigh, or buttocks that worsens with activity.
- Fatigue: A feeling of tiredness or heaviness in the legs that makes walking difficult.
- Numbness or Tingling: Sensations of pins and needles or loss of feeling in the affected area.
- Pain Relief with Rest: Discomfort that subsides within minutes of stopping physical activity.
- Cool Skin: The skin on the legs may feel cooler to the touch compared to other parts of the body.
When to Seek Medical Attention
While occasional muscle soreness is normal, persistent or worsening symptoms should prompt a visit to a healthcare provider. Individuals experiencing severe pain, discoloration of the legs, or open sores that do not heal should seek immediate medical care, as these could indicate advanced stages of peripheral artery disease or other serious conditions.
Treatment Options for Leg Pain While Walking
The treatment approach for leg pain while walking depends on the underlying cause and severity of the condition. In many cases, lifestyle modifications and conservative therapies can provide significant relief.
Lifestyle Changes
Making healthy lifestyle choices is often the first step in managing leg pain while walking. These changes not only address the symptoms but also help prevent further progression of the condition.
- Regular Exercise: Engaging in low-impact activities such as walking, swimming, or cycling can improve circulation and strengthen the muscles.
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall cardiovascular health.
- Smoking Cessation: Smoking damages blood vessels and accelerates the progression of peripheral artery disease. Quitting smoking is one of the most effective ways to reduce symptoms.
- Weight Management: Maintaining a healthy weight reduces stress on the legs and improves blood flow.
Medications
In addition to lifestyle changes, medications may be prescribed to manage symptoms and improve blood flow. Commonly used drugs include:
- Antiplatelet Agents: Medications such as aspirin or clopidogrel help prevent blood clots and improve circulation.
- Cholesterol-Lowering Drugs: Statins are often prescribed to reduce plaque buildup in the arteries.
- Blood Pressure Medications: Controlling high blood pressure can alleviate stress on the circulatory system.
- Pain Relievers: Over-the-counter pain medications may provide temporary relief for mild to moderate discomfort.
Physical Therapy
Physical therapy plays an important role in strengthening the muscles and improving endurance. A trained therapist can design a personalized exercise program tailored to the individual’s needs and abilities. Supervised treadmill workouts, resistance training, and stretching exercises are commonly included in these programs.
Minimally Invasive Procedures
For individuals with severe symptoms unresponsive to conservative treatments, minimally invasive procedures may be recommended. These interventions aim to restore proper blood flow and alleviate pain.
- Angioplasty: A small balloon is inserted into the affected artery and inflated to widen the passage and improve blood flow.
- Stent Placement: A metal mesh tube is placed in the artery to keep it open and prevent future blockages.
- Atherectomy: This procedure involves removing plaque buildup from the walls of the arteries using specialized tools.
Surgical Interventions
In rare cases where non-surgical treatments fail, surgery may be necessary. Bypass surgery, for example, reroutes blood flow around blocked arteries using a graft. While surgical options carry higher risks, they can provide long-term relief for those with advanced disease.
Preventive Measures
Preventing leg pain while walking involves adopting habits that promote vascular health and reduce the risk of developing circulatory issues. Some key strategies include:
- Regular Check-Ups: Routine visits to a healthcare provider allow for early detection and management of potential problems.
- Foot Care: Proper foot hygiene and regular inspections help prevent infections and complications, particularly in individuals with diabetes.
- Stress Reduction: Managing stress through techniques such as meditation or yoga supports overall well-being and cardiovascular health.
Educating Yourself and Others
Raising awareness about leg pain while walking and its potential implications is vital for promoting early intervention. Encouraging loved ones to pay attention to their bodies and seek medical advice when needed can make a significant difference in outcomes.