Lactose intolerance, often abbreviated as LI, is a common digestive condition that affects millions of people worldwide. It occurs when the body has difficulty digesting lactose, a sugar found in milk and dairy products. While it is not life-threatening, lactose intolerance can significantly impact an individual’s quality of life if not managed properly. This article explores the causes, symptoms, and effective strategies for managing this condition.
Understanding Lactose Intolerance
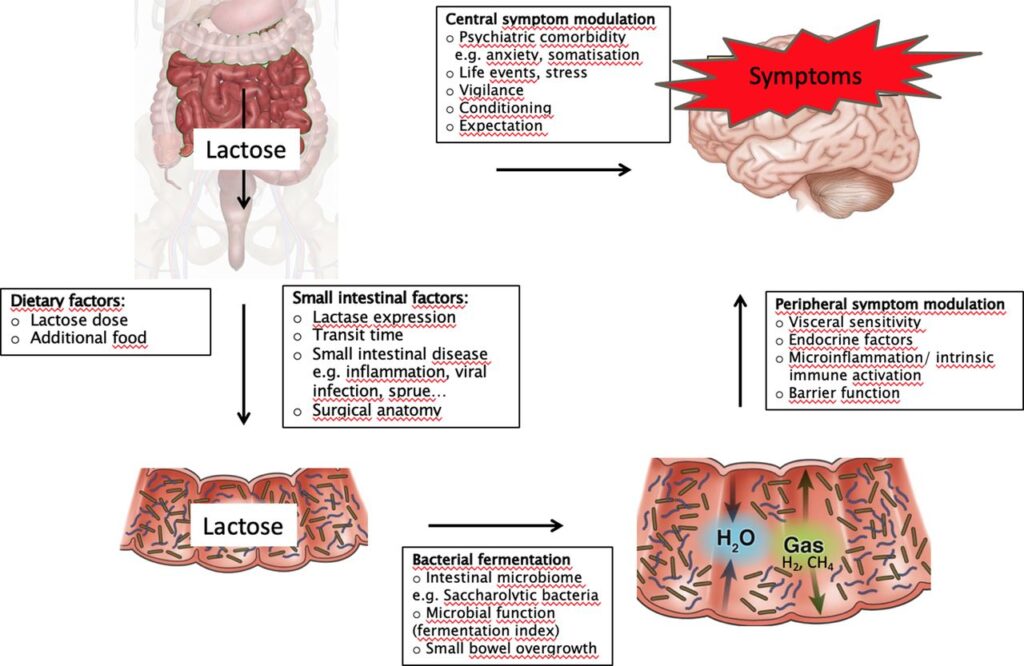
Lactose intolerance arises when the small intestine does not produce enough of an enzyme called lactase. Lactase is responsible for breaking down lactose into simpler sugars, such as glucose and galactose, which can then be absorbed into the bloodstream. Without sufficient lactase, undigested lactose moves into the colon, where it interacts with bacteria and leads to various uncomfortable symptoms.
Types of Lactose Intolerance
There are several types of lactose intolerance, each with its own underlying cause:
- Primary Lactose Intolerance: This is the most common type and typically develops in adulthood. It occurs due to a natural decline in lactase production as people age, especially in populations where dairy consumption is not historically prevalent.
- Secondary Lactose Intolerance: This form results from an injury or illness affecting the small intestine, such as celiac disease, Crohn’s disease, or infections like gastroenteritis. In these cases, the production of lactase is temporarily reduced.
- Congenital Lactose Intolerance: A rare genetic condition where infants are born without the ability to produce lactase. This type is inherited in an autosomal recessive pattern.
- Developmental Lactose Intolerance: Some premature babies may experience temporary lactose intolerance because their digestive systems are not fully developed at birth.
Causes of Lactose Intolerance
The primary cause of lactose intolerance is insufficient production of the enzyme lactase. However, several factors can contribute to this deficiency:
Genetic Factors
In many cases, lactose intolerance is linked to genetics. Populations with a historical reliance on dairy farming, such as those in Northern Europe, tend to have lower rates of lactose intolerance. Conversely, individuals of East Asian, African, and Native American descent are more likely to develop lactose intolerance due to genetic predisposition.
Age-Related Decline
As people grow older, their bodies naturally produce less lactase. This decline begins after childhood and continues into adulthood, making older adults more susceptible to lactose intolerance.
Intestinal Damage
Conditions that damage the lining of the small intestine can impair lactase production. Diseases like celiac disease and inflammatory bowel disease, as well as surgeries involving the digestive tract, can lead to secondary lactose intolerance.
Infections
Gastrointestinal infections, particularly in children, can temporarily reduce lactase production. While most cases resolve on their own, some individuals may experience long-term effects.
Symptoms of Lactose Intolerance
The symptoms of lactose intolerance can vary in severity and typically appear within a few hours of consuming dairy products. Common symptoms include:
Bloating
Bloating is one of the most frequent complaints among individuals with lactose intolerance. The undigested lactose ferments in the colon, producing gas and causing the abdomen to feel swollen and uncomfortable.
Diarrhea
Diarrhea occurs when the osmotic pressure of undigested lactose draws water into the colon. This symptom is particularly common in children with lactose intolerance.
Gas
The fermentation of lactose by gut bacteria produces gases like hydrogen, methane, and carbon dioxide. Excessive gas buildup can lead to flatulence and discomfort.
Abdominal Pain
Cramping and abdominal pain are common symptoms caused by the combination of bloating, gas, and diarrhea. The severity of the pain can range from mild to severe, depending on the amount of lactose consumed.
Nausea
Some individuals may experience nausea or even vomiting after consuming lactose-containing foods. This symptom is less common but can occur in more severe cases.
Diagnosing Lactose Intolerance
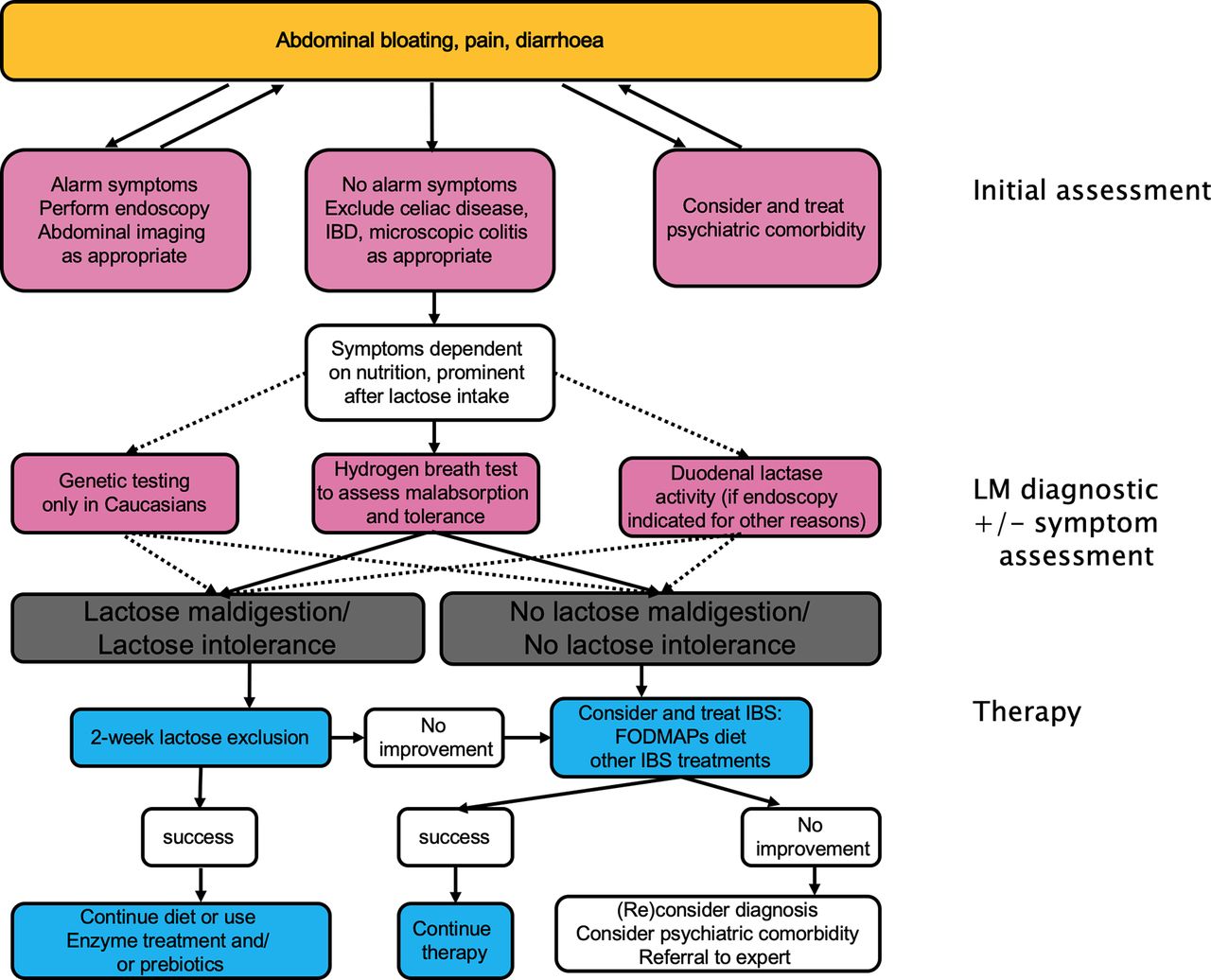
Diagnosing lactose intolerance involves a combination of medical history evaluation, physical examination, and diagnostic tests. Healthcare providers may use the following methods to confirm the condition:
Lactose Tolerance Test
This test measures blood glucose levels before and after consuming a lactose-rich drink. If the body cannot digest lactose properly, blood glucose levels will not rise as expected.
Hydrogen Breath Test
During this test, the patient consumes a lactose solution, and their breath is analyzed for hydrogen levels. Elevated hydrogen indicates that undigested lactose is being fermented in the colon.
Stool Acidity Test
This test is primarily used for infants and young children. It detects lactic acid and other fermentation byproducts in the stool, which are signs of lactose malabsorption.
Managing Lactose Intolerance
While there is no cure for lactose intolerance, it can be effectively managed through dietary adjustments and lifestyle changes. Here are some strategies to help individuals cope with the condition:
Dietary Modifications
One of the most effective ways to manage lactose intolerance is to limit or avoid foods and beverages containing lactose. These include:
- Milk and cream
- Cheese, especially soft varieties
- Ice cream
- Yogurt
- Processed foods with hidden lactose, such as baked goods and salad dressings
Reading food labels carefully is essential to identify lactose-containing ingredients.
Lactase Supplements
Over-the-counter lactase enzyme supplements can help individuals digest lactose more effectively. These supplements are available in tablet or liquid form and should be taken just before consuming dairy products.
Lactose-Free Products
Many supermarkets now offer lactose-free versions of milk, cheese, and yogurt. These products are treated with lactase to break down the lactose, making them easier to digest.
Alternative Sources of Calcium
Since dairy products are a primary source of calcium, individuals with lactose intolerance need to find alternative sources to maintain bone health. Good options include:
- Leafy green vegetables like kale and spinach
- Fortified plant-based milks, such as almond, soy, or oat milk
- Tofu
- Nuts and seeds
- Fish with edible bones, such as sardines
Gradual Reintroduction
Some individuals with lactose intolerance may tolerate small amounts of lactose without experiencing symptoms. Gradually reintroducing dairy products in small portions can help determine personal tolerance levels.
Living with Lactose Intolerance
While lactose intolerance requires ongoing management, it does not have to restrict one’s enjoyment of food or social activities. With careful planning and awareness, individuals can lead healthy, fulfilling lives while minimizing discomfort. Experimenting with recipes, exploring new ingredients, and staying informed about nutritional needs are all valuable steps toward thriving with lactose intolerance.