Keratoconus, often abbreviated as KC, is a progressive eye condition that affects the structure of the cornea, leading to distorted vision. While it may sound complex, understanding this disorder is crucial for those who experience its symptoms or know someone who does. In this article, we will delve into what keratoconus is, its causes, symptoms, diagnosis, and available treatment options.
What Is Keratoconus?
Keratoconus is an eye disorder characterized by the thinning and bulging of the cornea, the clear, dome-shaped front surface of the eye. Normally, the cornea has a smooth, rounded shape that helps focus light onto the retina, enabling clear vision. However, in individuals with this condition, the cornea gradually becomes cone-shaped, causing blurred and distorted vision.
This change in the cornea’s shape can lead to significant visual impairment, making daily tasks like reading, driving, or recognizing faces challenging. The progression of the condition varies from person to person, with some experiencing mild changes and others facing severe vision loss.
Causes of Keratoconus
The exact cause of keratoconus remains unknown, but researchers believe it results from a combination of genetic, environmental, and biological factors. Below are some potential contributors:
Genetic Factors
- Studies suggest that keratoconus may run in families, indicating a genetic predisposition. If a close family member has the condition, there is an increased likelihood of developing it.
Environmental Influences
- Frequent eye rubbing, especially in individuals with allergies or conditions like asthma, may weaken the corneal tissue over time, contributing to the development of keratoconus.
- Exposure to ultraviolet light and oxidative stress may also play a role in damaging the corneal cells.
Hormonal Changes
- Some studies have linked hormonal changes during puberty or pregnancy to the onset or progression of keratoconus, though more research is needed to confirm this connection.
Symptoms of Keratoconus
The symptoms of keratoconus typically begin in adolescence or early adulthood and progress gradually over time. Early detection is key to managing the condition effectively. Common symptoms include:
- Blurred or distorted vision
- Increased sensitivity to light and glare
- Frequent changes in eyeglass prescriptions
- Difficulty seeing at night
- Halos or streaks around lights
- Double vision in one eye
It is important to note that these symptoms can overlap with other eye conditions, so consulting an eye care professional is essential for an accurate diagnosis.
Diagnosing Keratoconus
Diagnosing keratoconus requires a comprehensive eye examination. Eye care professionals use several tests and tools to assess the shape and health of the cornea. These diagnostic methods include:
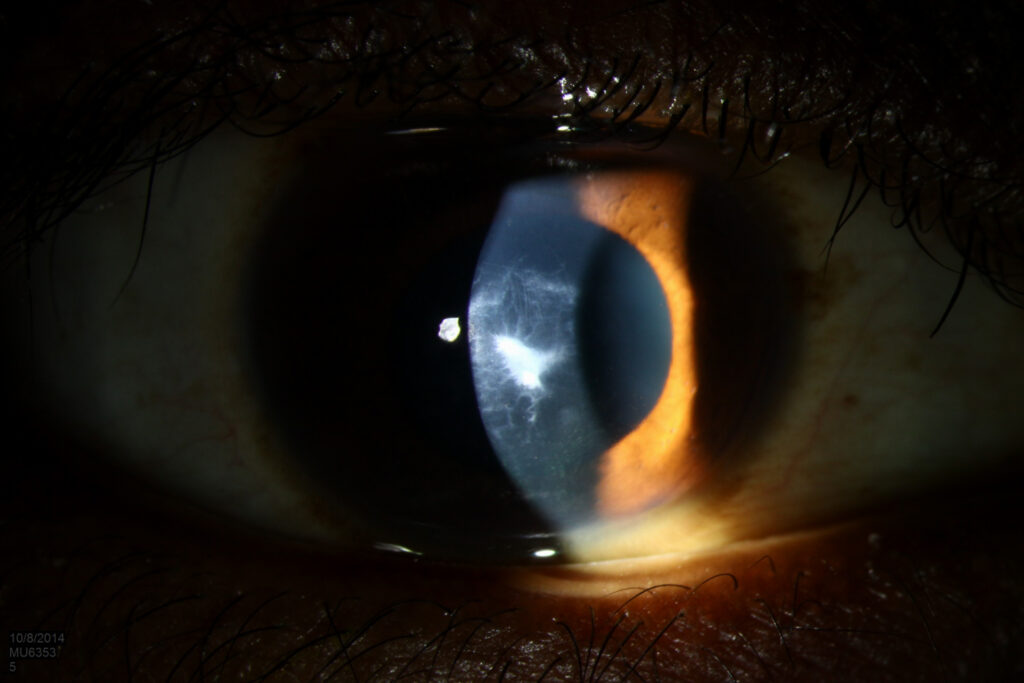
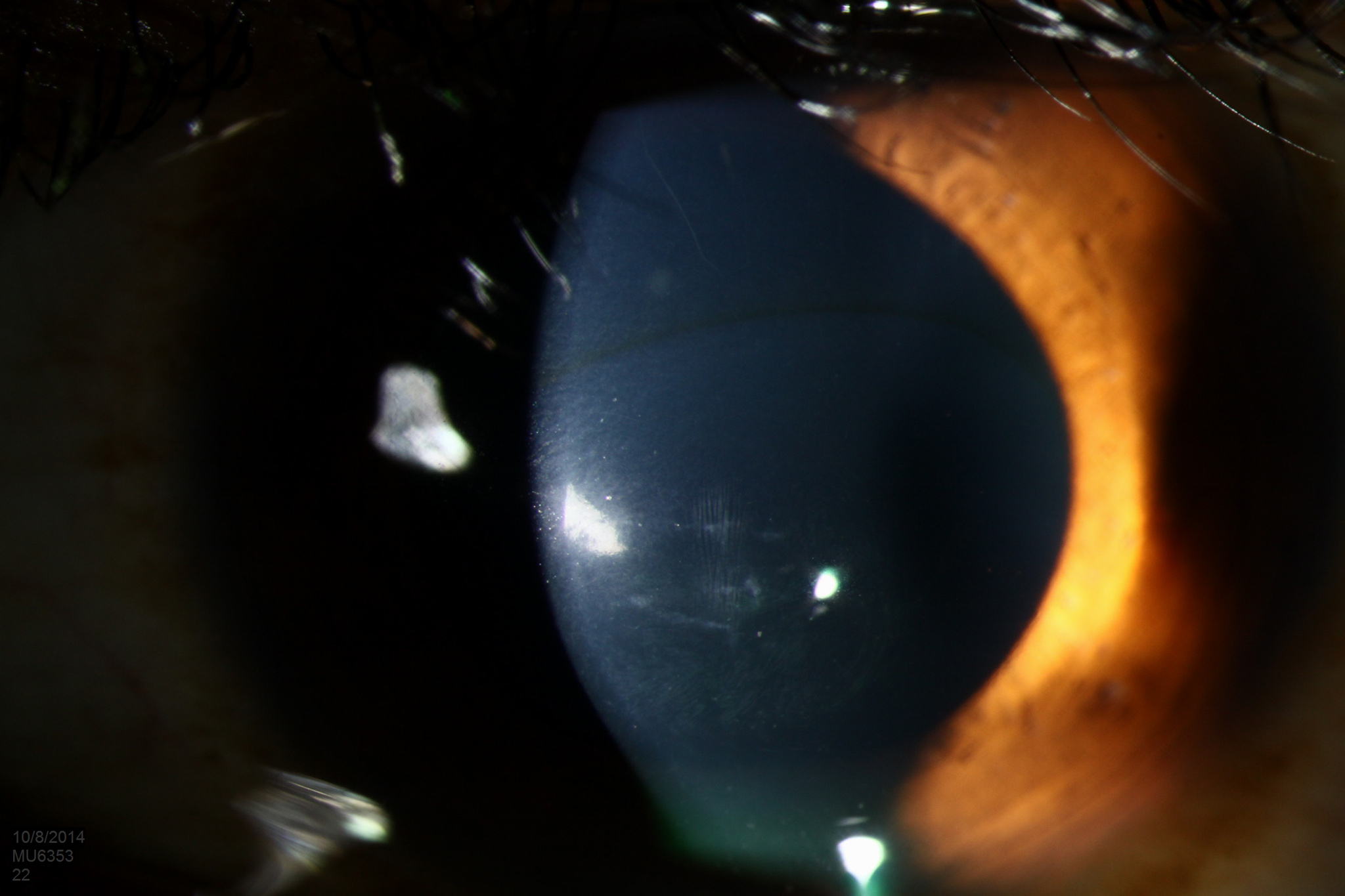
Slit Lamp Examination
A slit lamp is a specialized microscope that allows the doctor to examine the cornea in detail. It can reveal signs of thinning or bulging in the corneal tissue.
Corneal Topography
This non-invasive imaging test creates a detailed map of the cornea’s surface. It helps identify irregularities in the corneal shape, such as steepening or asymmetry, which are characteristic of keratoconus.
Keratometry
Keratometry measures the curvature of the cornea. Abnormal readings may indicate the presence of keratoconus.
Pachymetry
This test measures the thickness of the cornea. Thinning of the corneal tissue is a hallmark of keratoconus and can be detected using pachymetry.
Treatment Options for Keratoconus
While there is no cure for keratoconus, several treatment options are available to manage the condition and improve vision. The choice of treatment depends on the severity of the condition and how quickly it progresses.
Corrective Lenses
In the early stages of keratoconus, corrective lenses such as glasses or soft contact lenses may be sufficient to correct mild vision problems. As the condition progresses, specialized contact lenses may be required.
Rigid Gas Permeable Lenses
These hard contact lenses provide a smooth surface to compensate for the irregular shape of the cornea, improving vision significantly.
Scleral Lenses
Scleral lenses are larger than traditional contact lenses and rest on the white part of the eye, known as the sclera. They create a tear-filled vault over the cornea, offering comfort and better vision for individuals with advanced keratoconus.
Cross-Linking Procedure
Corneal cross-linking is a minimally invasive procedure designed to strengthen the corneal tissue and prevent further progression of keratoconus. During the procedure, riboflavin (vitamin B2) eye drops are applied to the cornea, followed by exposure to ultraviolet light. This process promotes the formation of new bonds between collagen fibers in the cornea, enhancing its stability.
Intracorneal Ring Segments
Also known as corneal inserts, intracorneal ring segments are small, crescent-shaped devices implanted into the cornea to flatten its surface and improve vision. This option is suitable for individuals with moderate keratoconus who do not respond well to contact lenses.
Corneal Transplant
In severe cases where other treatments fail, a corneal transplant may be necessary. During this surgical procedure, the damaged corneal tissue is replaced with healthy donor tissue. While effective, corneal transplants require a lengthy recovery period and lifelong follow-up care.
Living with Keratoconus
Managing keratoconus involves regular monitoring and adapting to changes in vision over time. Here are some tips for living with the condition:
- Schedule routine eye exams to track the progression of the condition and adjust treatment plans accordingly.
- Avoid excessive eye rubbing, as it can worsen the thinning of the cornea.
- Work closely with an eye care professional to find the most comfortable and effective corrective lenses.
- Educate yourself about the latest advancements in keratoconus treatment to explore all available options.
Research and Future Directions
Ongoing research aims to uncover the underlying mechanisms of keratoconus and develop innovative treatments. Scientists are exploring gene therapies, advanced imaging techniques, and novel surgical approaches to address the root causes of the condition. Additionally, efforts are underway to improve the accessibility and affordability of existing treatments, ensuring that individuals with keratoconus receive the care they need.
Artificial Intelligence in Diagnosis
Recent advancements in artificial intelligence have shown promise in enhancing the accuracy and efficiency of diagnosing keratoconus. Machine learning algorithms can analyze corneal topography data to detect subtle changes that might be missed during a manual examination.
Biological Therapies
Researchers are investigating the potential of stem cell therapy and tissue engineering to regenerate damaged corneal tissue. These cutting-edge approaches could revolutionize the way keratoconus is treated in the future.