Keratitis, often abbreviated as “K,” is an inflammation of the cornea, the clear front part of the eye. This condition can affect vision and, if left untreated, may lead to serious complications. Understanding the causes, symptoms, diagnostic methods, and treatment options for this condition is essential for maintaining good eye health.
What is Keratitis?
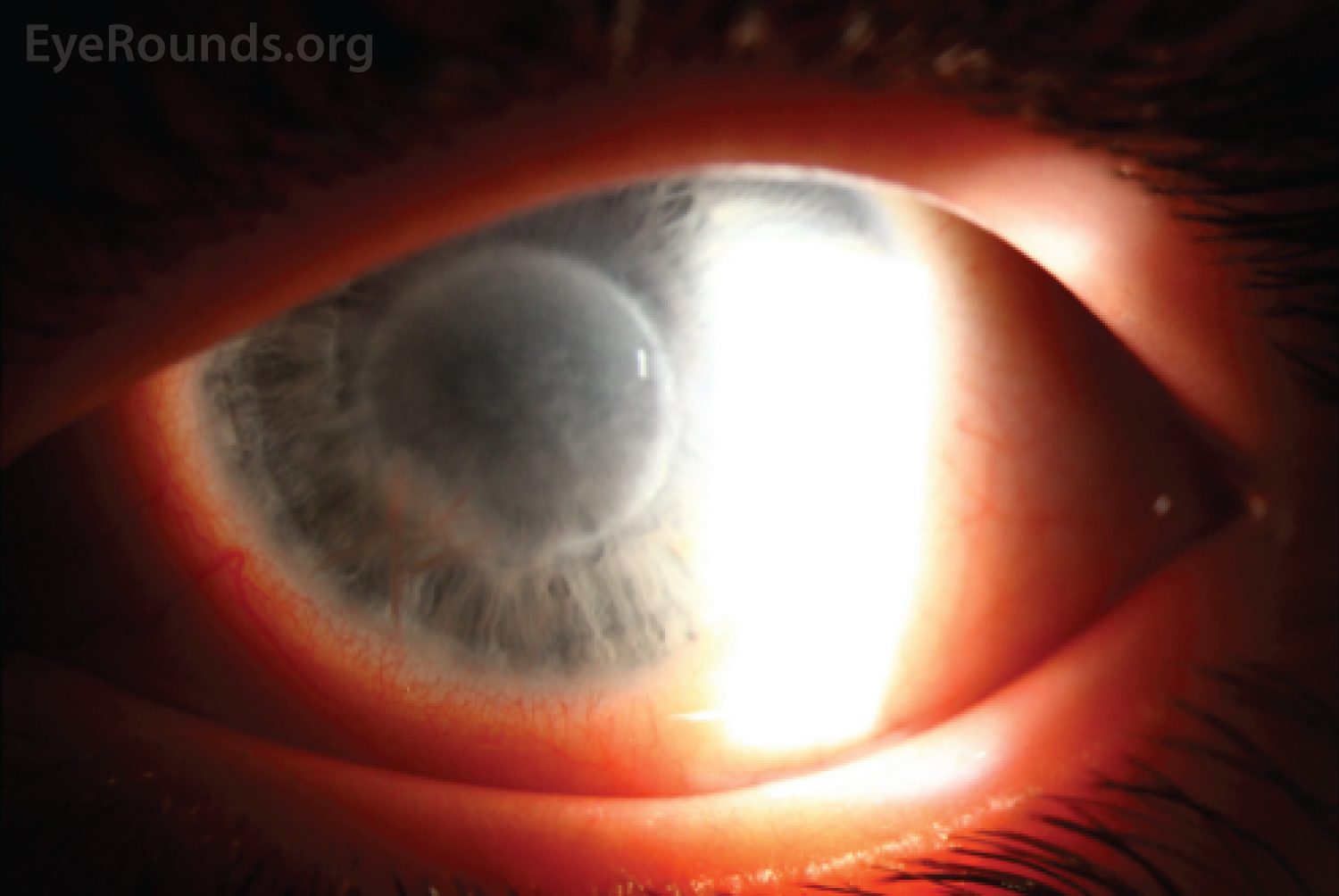
Keratitis refers to the inflammation of the cornea, which is the transparent layer that covers the front of the eye. The cornea plays a crucial role in focusing vision, and any damage or infection to this area can significantly impact eyesight. Keratitis can be caused by various factors, including infections, injuries, and underlying medical conditions.
Causes of Keratitis
The causes of keratitis can be broadly categorized into infectious and non-infectious types. Below are some common causes:
Infectious Causes
- Bacterial Infections: Bacteria such as Staphylococcus aureus and Pseudomonas aeruginosa can invade the cornea, leading to bacterial keratitis. This type of infection is more common in people who wear contact lenses improperly or do not maintain proper hygiene.
- Viral Infections: Herpes simplex virus and varicella-zoster virus are two common viral agents that can cause keratitis. Viral keratitis often recurs and requires long-term management.
- Fungal Infections: Fungi like Aspergillus and Fusarium can cause fungal keratitis, especially in individuals with weakened immune systems or those exposed to plant material or soil.
- Parasitic Infections: Acanthamoeba, a microscopic parasite found in water, can cause a severe form of keratitis, particularly in contact lens users who swim or shower while wearing their lenses.
Non-Infectious Causes
- Trauma or Injury: Any injury to the cornea, such as scratches or abrasions, can lead to inflammation and subsequent keratitis.
- Allergic Reactions: Allergens like pollen, dust, or animal dander can irritate the eyes and cause allergic keratitis.
- Dry Eye Syndrome: Insufficient tear production or poor-quality tears can result in chronic irritation and inflammation of the cornea.
- Contact Lens Overuse: Wearing contact lenses for extended periods without proper cleaning or disinfection increases the risk of developing keratitis.
Symptoms of Keratitis
The symptoms of keratitis can vary depending on the underlying cause and severity of the condition. Common signs and symptoms include:
- Eye redness
- Pain or discomfort in the eye
- Blurred or decreased vision
- Sensitivity to light (photophobia)
- Excessive tearing or discharge from the eye
- A feeling of something being stuck in the eye (foreign body sensation)
- Swelling around the eye
If you experience any of these symptoms, it is important to seek medical attention promptly to prevent further complications.
Diagnosis of Keratitis
Diagnosing keratitis involves a thorough examination of the eye and may require specific tests to determine the underlying cause. Here are some common diagnostic steps:
Medical History and Physical Examination
An eye care professional will begin by asking about your medical history, including any recent eye injuries, contact lens use, or exposure to potential irritants. They will then perform a physical examination of the eye using specialized tools such as a slit lamp, which provides a magnified view of the cornea and surrounding structures.
Laboratory Tests
In cases where an infection is suspected, the doctor may take a sample of the affected tissue or fluid from the eye for laboratory analysis. These tests help identify the specific bacteria, virus, fungus, or parasite causing the infection, allowing for targeted treatment.
Corneal Staining
To detect any damage or abnormalities on the surface of the cornea, the doctor may apply a special dye called fluorescein to the eye. When viewed under a blue light, the dye highlights areas of the cornea that are damaged or inflamed.
Other Imaging Techniques
In rare cases, advanced imaging techniques such as confocal microscopy or optical coherence tomography may be used to get a detailed view of the corneal layers and assess the extent of inflammation or scarring.
Treatment Options for Keratitis
The treatment for keratitis depends on its underlying cause. Early diagnosis and appropriate treatment are critical to prevent complications such as corneal scarring or vision loss. Below are some common treatment approaches:
Treatment for Infectious Keratitis
- Bacterial Keratitis: Antibiotic eye drops or ointments are typically prescribed to treat bacterial infections. In severe cases, oral antibiotics may also be necessary.
- Viral Keratitis: Antiviral medications, either in the form of eye drops or oral tablets, are used to manage viral infections. Recurrent cases may require long-term antiviral therapy.
- Fungal Keratitis: Antifungal eye drops or oral medications are used to treat fungal infections. This type of keratitis can be challenging to treat and may require prolonged therapy.
- Parasitic Keratitis: Treatment for Acanthamoeba keratitis involves specific antimicrobial eye drops and sometimes oral medications. This condition often requires aggressive and lengthy treatment.
Treatment for Non-Infectious Keratitis
- Trauma-Related Keratitis: Mild cases of trauma-induced keratitis may resolve on their own with the use of lubricating eye drops and avoiding further irritation. More severe cases may require antibiotic or anti-inflammatory medications.
- Allergic Keratitis: Avoiding allergens and using antihistamine eye drops can help alleviate symptoms. In some cases, corticosteroid eye drops may be prescribed to reduce inflammation.
- Dry Eye-Related Keratitis: Artificial tears, gels, or ointments can help keep the eyes moist. In more severe cases, prescription medications or procedures to increase tear production may be necessary.
- Contact Lens-Induced Keratitis: Discontinuing contact lens use temporarily and switching to glasses is often recommended. Proper lens hygiene and care should be emphasized to prevent recurrence.
Surgical Interventions
In cases where keratitis leads to significant corneal scarring or vision impairment, surgical interventions may be required. Procedures such as corneal transplantation or laser surgery may be considered to restore vision and improve eye health.
Preventive Measures
Preventing keratitis involves adopting good eye care practices and minimizing exposure to risk factors. Some preventive measures include:
- Washing hands thoroughly before handling contact lenses
- Disinfecting contact lenses properly and replacing them as recommended
- Avoiding sleeping or swimming while wearing contact lenses
- Using protective eyewear when engaging in activities that pose a risk of eye injury
- Managing underlying conditions like dry eye syndrome or allergies effectively
By following these preventive strategies, individuals can reduce their risk of developing keratitis and maintain healthy eyes.





