Kawasaki Disease, often abbreviated as KD, is a rare but serious condition that primarily affects children under the age of five. It is characterized by inflammation of the blood vessels throughout the body, which can lead to complications if left untreated. This article delves into the causes, symptoms, diagnosis, and treatment options for this enigmatic illness, shedding light on its complexities and offering guidance for parents, caregivers, and healthcare providers.

Understanding Kawasaki Disease
Kawasaki Disease was first identified in Japan in 1967 by Dr. Tomisaku Kawasaki. Since then, it has been recognized worldwide, though its exact cause remains unknown. The disease predominantly affects young children, with boys being slightly more susceptible than girls. While most cases occur in children under five years old, older children and even adults can occasionally develop the condition.
Possible Causes
The precise cause of Kawasaki Disease is still a mystery, but researchers believe it may result from an abnormal immune response triggered by an infection or environmental factor. Some studies suggest that genetic predisposition might play a role, as certain populations, such as those of Asian descent, appear to be at higher risk. However, no definitive evidence points to a single infectious agent or environmental trigger responsible for the disease.
- Infectious Agents: Some theories propose that viruses or bacteria could initiate the inflammatory process seen in Kawasaki Disease. However, no specific pathogen has been consistently linked to the condition.
- Immune System Response: The immune system’s overreaction to an unknown stimulus is thought to contribute to the widespread inflammation observed in affected individuals.
- Environmental Factors: Seasonal patterns and geographic clustering suggest that environmental factors, such as exposure to pollutants or allergens, might influence the onset of the disease.
Symptoms of Kawasaki Disease
Kawasaki Disease manifests through a variety of symptoms that typically develop in phases. Early recognition of these signs is crucial for timely intervention and preventing potential complications.
Phase 1: Acute Phase
The acute phase usually lasts one to two weeks and is marked by high fever and other systemic symptoms. Key indicators during this stage include:
- Prolonged Fever: A persistent high fever lasting five days or more is one of the hallmark signs of Kawasaki Disease.
- Rash: A red, blotchy rash often appears on the trunk and may spread to other parts of the body.
- Swollen Lymph Nodes: Enlarged lymph nodes, particularly in the neck, are common.
- Red Eyes: Conjunctivitis without discharge (redness of the whites of the eyes) is frequently observed.
- Changes in Mouth and Lips: Cracked lips, a strawberry-like appearance of the tongue, and redness inside the mouth are typical.
- Swollen Hands and Feet: The palms and soles may become red and swollen, sometimes accompanied by peeling skin later in the course of the disease.
Phase 2: Subacute Phase
During the subacute phase, which occurs about two weeks after the onset of symptoms, the fever begins to subside, but new issues may arise:
- Peeling Skin: Large sheets of skin may peel off the hands and feet.
- Joint Pain: Some children experience joint pain or arthritis-like symptoms.
- Gastrointestinal Problems: Abdominal pain, vomiting, or diarrhea may occur.
Phase 3: Convalescent Phase
The convalescent phase begins several weeks after the initial symptoms and can last up to eight weeks. During this time, the child gradually recovers, and physical signs improve. However, close monitoring is essential to detect any lingering effects on the heart or blood vessels.
Diagnosing Kawasaki Disease
Diagnosing Kawasaki Disease can be challenging because its symptoms mimic those of other childhood illnesses, such as measles, scarlet fever, or juvenile rheumatoid arthritis. There is no single test to confirm the presence of the disease; instead, doctors rely on clinical criteria and laboratory findings.
Clinical Criteria
To diagnose Kawasaki Disease, a physician looks for the presence of at least five key symptoms:
- Fever lasting five or more days
- Rash
- Conjunctival injection (red eyes)
- Changes in the mouth, lips, or throat
- Swelling or redness of the hands and feet
- Enlarged lymph nodes in the neck
If a child exhibits four out of the six criteria, along with prolonged fever, a diagnosis of Kawasaki Disease is strongly considered. Incomplete cases, where fewer symptoms are present, require additional testing and evaluation.
Laboratory Tests
Blood tests and imaging studies help support the diagnosis and assess potential complications:
- Blood Tests: Elevated white blood cell count, anemia, and increased levels of inflammatory markers like C-reactive protein indicate systemic inflammation.
- Echocardiogram: An ultrasound of the heart checks for coronary artery abnormalities, which are a major concern in Kawasaki Disease.
Treatment Options for Kawasaki Disease
Early treatment is critical to reducing the risk of complications, particularly damage to the coronary arteries. The primary goal of therapy is to reduce inflammation and prevent long-term cardiovascular problems.
Intravenous Immunoglobulin (IVIG)
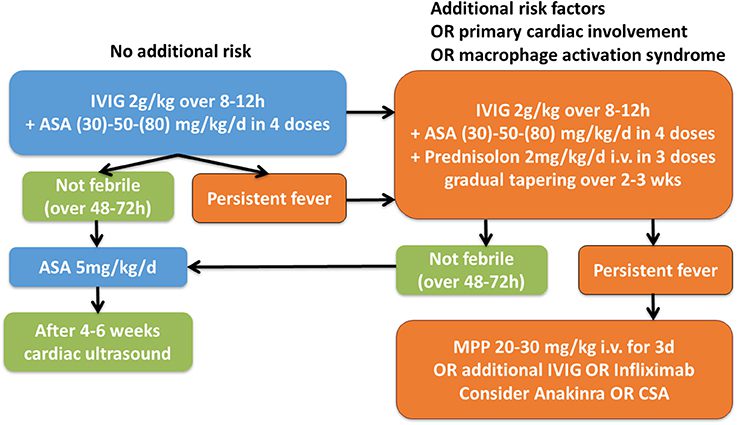
Intravenous immunoglobulin is the cornerstone of treatment for Kawasaki Disease. Administered within ten days of symptom onset, IVIG helps suppress the immune response and reduces the likelihood of coronary artery involvement. Most children respond well to this treatment, with their fever subsiding within 48 hours.
Aspirin Therapy
High doses of aspirin are given initially to manage inflammation and fever. Once the fever resolves, the dosage is lowered to prevent blood clots and protect the heart. Aspirin therapy continues until follow-up tests confirm normal heart function.
Additional Treatments
In cases where intravenous immunoglobulin does not adequately control symptoms, additional treatments may be necessary:
- Corticosteroids: Steroids may be prescribed to further reduce inflammation when IVIG alone is insufficient.
- Biologic Agents: Medications targeting specific components of the immune system, such as tumor necrosis factor inhibitors, are sometimes used in refractory cases.
Monitoring and Follow-Up
Regular follow-up appointments are essential to monitor recovery and screen for any delayed complications. Echocardiograms are performed periodically to evaluate the health of the coronary arteries. Children who develop coronary artery aneurysms require ongoing cardiology care to manage their condition effectively.
Prevention and Outlook
While there is currently no known way to prevent Kawasaki Disease, early diagnosis and prompt treatment significantly improve outcomes. With appropriate medical care, most children recover fully and do not experience long-term effects. However, vigilance is required to identify and address any residual cardiac issues.
Research into the causes and optimal management of Kawasaki Disease continues, offering hope for better understanding and improved therapies in the future. Parents and caregivers are encouraged to seek immediate medical attention if they notice symptoms consistent with this condition, ensuring the best possible outcome for affected children.