Iron overload disorder, commonly referred to as hemochromatosis, is a medical condition characterized by excessive accumulation of iron in the body. This buildup of iron can lead to serious health complications if left untreated. Hemochromatosis affects various organs, including the liver, heart, and pancreas, and may result in organ damage or failure. Understanding the causes, symptoms, diagnosis, and management of this condition is crucial for early detection and effective treatment.
What is Iron Overload Disorder?
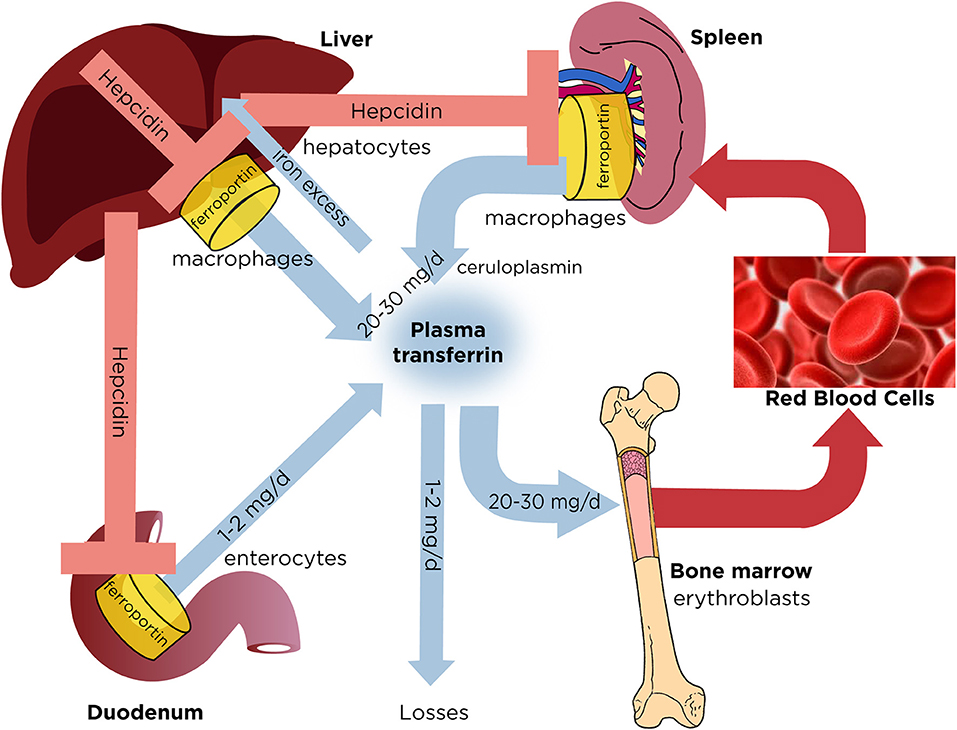
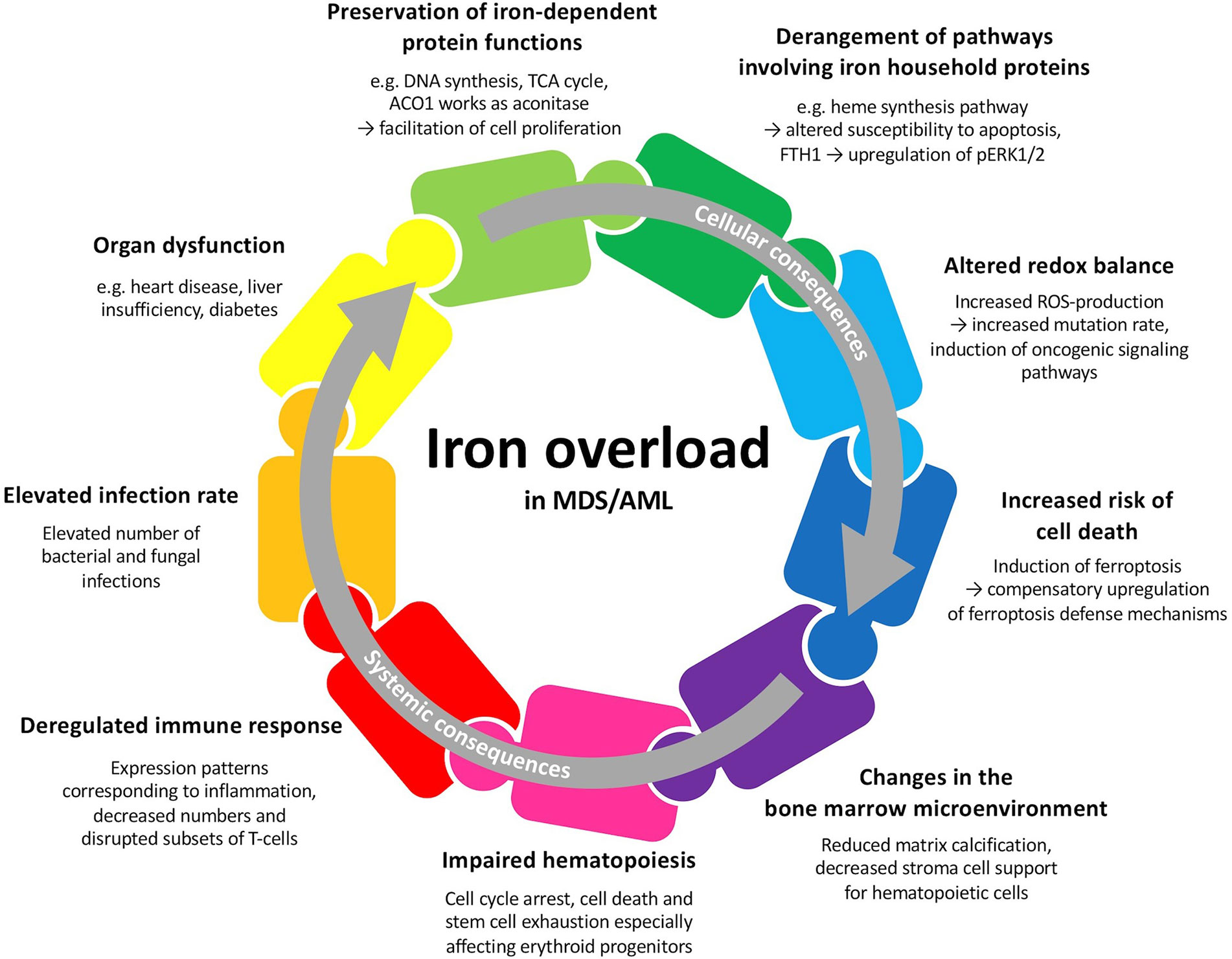
Iron overload disorder occurs when the body absorbs too much iron from the diet. Normally, the body regulates iron levels carefully, but in individuals with this condition, the regulation mechanism malfunctions. The excess iron accumulates in tissues and organs, leading to inflammation, scarring, and eventually organ dysfunction. There are two main types of iron overload disorders: primary hemochromatosis, which is genetic, and secondary hemochromatosis, which arises from other underlying conditions.
Primary Hemochromatosis
Primary hemochromatosis is an inherited condition caused by mutations in specific genes. The most common form is linked to mutations in the HFE gene, which plays a role in regulating iron absorption in the intestines. When this gene is defective, the body absorbs more iron than it needs, leading to iron overload over time.
Secondary Hemochromatosis
Secondary hemochromatosis is not inherited but rather develops as a result of other medical conditions or factors. These may include chronic liver disease, frequent blood transfusions, or excessive intake of iron supplements. People with certain blood disorders, such as thalassemia or sickle cell anemia, are also at higher risk of developing secondary hemochromatosis due to repeated blood transfusions.
Causes of Iron Overload Disorder
The causes of iron overload disorder vary depending on whether it is primary or secondary. Below are the primary factors contributing to each type:
Genetic Factors
- Mutations in the HFE gene are the most common cause of primary hemochromatosis. These mutations disrupt the body’s ability to regulate iron absorption.
- In rare cases, mutations in other genes, such as hemojuvelin, hepcidin, or transferrin receptor 2, can also lead to iron overload.
Underlying Medical Conditions
- Chronic liver diseases, such as hepatitis C or alcoholic liver disease, can impair the liver’s ability to process iron, leading to its accumulation.
- Blood disorders that require frequent blood transfusions can result in excessive iron levels in the body.
- Conditions like anemia or kidney failure may necessitate the use of iron supplements, which can contribute to iron overload if not monitored properly.
Lifestyle and Environmental Factors
- Excessive consumption of iron-rich foods or supplements without medical supervision can increase the risk of iron overload.
- Heavy alcohol consumption can exacerbate iron accumulation by damaging the liver and impairing its function.
Symptoms of Iron Overload Disorder
The symptoms of iron overload disorder often develop gradually and may not appear until later in life. In some cases, individuals may remain asymptomatic for years. Common symptoms include:
Early Symptoms
- Fatigue and weakness, which are often attributed to other causes.
- Joint pain, particularly in the hands and knees.
- Abdominal pain or discomfort, especially in the upper right quadrant where the liver is located.
Advanced Symptoms
- Darkening of the skin, giving it a bronze or gray appearance.
- Diabetes due to damage to the pancreas, which impairs insulin production.
- Irregular heartbeat or heart failure caused by iron deposits in the heart muscle.
- Liver cirrhosis or liver failure resulting from prolonged iron accumulation.
Gender-Specific Symptoms
- In women, irregular menstrual cycles or early menopause may occur due to hormonal imbalances caused by iron overload.
- In men, loss of libido or erectile dysfunction may be observed as a result of hormonal disturbances.
Diagnosis of Iron Overload Disorder
Diagnosing iron overload disorder involves a combination of clinical evaluation, laboratory tests, and imaging studies. Early diagnosis is essential to prevent complications and manage the condition effectively.
Clinical Evaluation
A healthcare provider will begin by taking a detailed medical history and conducting a physical examination. They will inquire about symptoms, family history of iron-related disorders, and any underlying medical conditions. During the physical exam, they may check for signs of iron overload, such as skin discoloration or enlarged liver.
Laboratory Tests
- Blood tests are used to measure serum ferritin levels, which indicate the amount of stored iron in the body. Elevated ferritin levels suggest iron overload.
- Transferrin saturation is another key test that measures the percentage of iron bound to transferrin, a protein that transports iron in the blood. High transferrin saturation levels are indicative of hemochromatosis.
- Genetic testing can identify mutations in the HFE gene or other genes associated with iron overload disorders.
Imaging Studies
- Liver biopsy may be performed to assess the extent of iron accumulation and liver damage. This procedure involves removing a small sample of liver tissue for analysis.
- Magnetic resonance imaging or MRI can provide non-invasive images of the liver and other organs to detect iron deposits.
Management of Iron Overload Disorder
Effective management of iron overload disorder focuses on reducing iron levels in the body and preventing complications. Treatment options depend on the severity of the condition and the underlying cause.
Phlebotomy
Phlebotomy, or therapeutic blood removal, is the most common treatment for primary hemochromatosis. During this procedure, a healthcare provider removes a pint of blood from the patient’s body, similar to donating blood. This process helps reduce iron levels by depleting the body’s iron stores. Phlebotomy is typically performed weekly or biweekly until iron levels return to normal. Maintenance phlebotomy may be required periodically to keep iron levels in check.
Iron Chelation Therapy
Iron chelation therapy is an alternative treatment for individuals who cannot undergo phlebotomy due to medical reasons, such as anemia or heart problems. This therapy involves the use of medications that bind to excess iron and facilitate its excretion through urine or stool. Commonly used chelating agents include deferoxamine, deferiprone, and deferasirox.
Dietary Modifications
Dietary changes can play a supportive role in managing iron overload disorder. Patients are advised to:
- Limit consumption of iron-rich foods, such as red meat, liver, and fortified cereals.
- Avoid vitamin C supplements, as they enhance iron absorption.
- Consume foods and beverages that inhibit iron absorption, such as tea, coffee, and calcium-rich foods.
Monitoring and Follow-Up
Regular monitoring is essential to ensure that iron levels remain within a safe range. Patients should undergo periodic blood tests to measure serum ferritin and transferrin saturation levels. Follow-up appointments with a healthcare provider allow for adjustments to the treatment plan as needed.
Treatment of Complications
If iron overload has already caused complications, such as diabetes, liver cirrhosis, or heart problems, additional treatments may be necessary. For example:
- Insulin therapy may be required to manage diabetes caused by pancreatic damage.
- Liver transplantation may be considered in cases of severe liver failure.
- Medications or procedures may be prescribed to address heart-related issues, such as arrhythmias or heart failure.
Prevention of Iron Overload Disorder
While primary hemochromatosis cannot be prevented due to its genetic nature, secondary hemochromatosis can often be avoided by addressing underlying causes. Preventive measures include:
- Regular screening for individuals with a family history of hemochromatosis.
- Monitoring iron levels in patients receiving frequent blood transfusions.
- Avoiding unnecessary iron supplements unless prescribed by a healthcare provider.
- Adopting a balanced diet and limiting alcohol consumption to protect liver health.
By understanding the causes, recognizing the symptoms, and adhering to proper management strategies, individuals with iron overload disorder can lead healthier lives and minimize the risk of complications.