Interstitial Lung Disease, often abbreviated as ILD, is a group of disorders that cause inflammation and scarring in the lungs. This condition affects the interstitium, which is the tissue and space around the air sacs of the lungs. Over time, this damage can make it difficult for the lungs to function properly, leading to breathing difficulties and reduced oxygen levels in the blood. In this article, we will explore the causes, symptoms, diagnosis, and care associated with this complex lung condition.
Understanding Interstitial Lung Disease
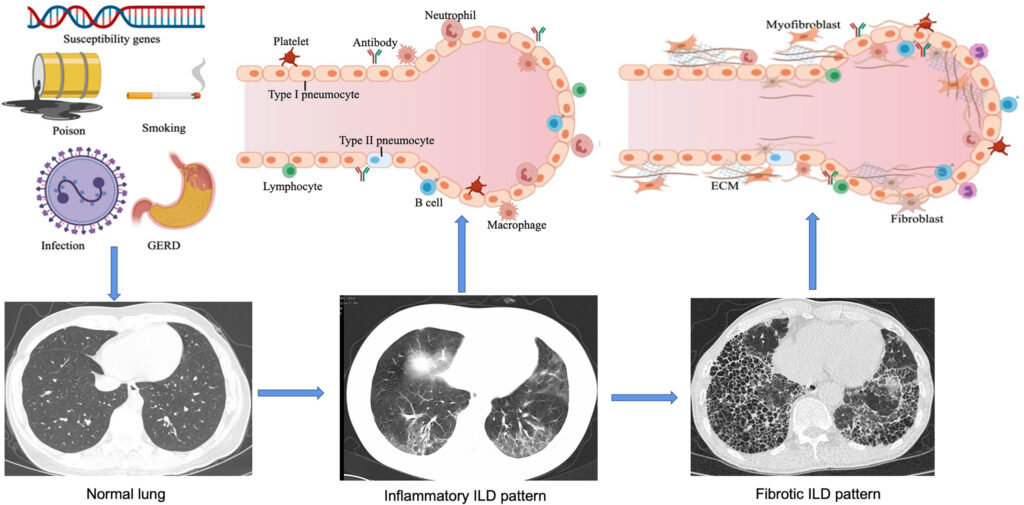
Interstitial Lung Disease encompasses a wide range of conditions that share similar characteristics. These diseases primarily affect the interstitium, a part of the lung that supports the tiny air sacs called alveoli. When the interstitium becomes inflamed or scarred, it interferes with the normal exchange of oxygen and carbon dioxide in the lungs. The result is a progressive decline in lung function, which can significantly impact a person’s quality of life.
Common Types of Interstitial Lung Disease
- Idiopathic Pulmonary Fibrosis: A chronic and progressive form of the disease with no known cause.
- Hypersensitivity Pneumonitis: Triggered by an allergic reaction to inhaled substances like mold or dust.
- Sarcoidosis: An inflammatory disease that can affect multiple organs, including the lungs.
- Rheumatoid Lung Disease: A complication of rheumatoid arthritis that affects the respiratory system.
- Occupational Lung Diseases: Caused by long-term exposure to harmful substances in the workplace.
Causes of Interstitial Lung Disease
The exact cause of interstitial lung disease varies depending on the specific type of condition. However, several factors are commonly associated with its development:
Environmental and Occupational Factors
Long-term exposure to certain environmental or occupational hazards can lead to lung damage. These include:
- Dust from coal, asbestos, or silica
- Fumes from chemicals or welding
- Bird droppings or mold spores
People working in industries such as mining, construction, or agriculture are at higher risk of developing these conditions due to prolonged exposure to harmful particles.
Autoimmune Disorders
Some autoimmune diseases can attack the lungs, causing inflammation and scarring. Examples include:
- Rheumatoid arthritis
- Lupus
- Scleroderma
In these cases, the immune system mistakenly targets healthy lung tissue, leading to progressive damage over time.
Medications and Treatments
Certain medications and treatments can also contribute to the development of interstitial lung disease. These include:
- Chemotherapy drugs used to treat cancer
- Antibiotics like nitrofurantoin
- Heart medications such as amiodarone
Prolonged use of these substances may increase the risk of lung damage, especially in individuals who already have underlying health issues.
Unknown Causes
In some cases, the exact cause of interstitial lung disease remains unknown. This is particularly true for idiopathic pulmonary fibrosis, where no clear trigger can be identified despite extensive testing and evaluation.
Symptoms of Interstitial Lung Disease
The symptoms of interstitial lung disease often develop gradually and worsen over time. Early detection is crucial for managing the condition effectively. Common symptoms include:
Shortness of Breath
One of the earliest and most noticeable symptoms is difficulty breathing, especially during physical activity. As the disease progresses, shortness of breath may occur even at rest.
Dry Cough
A persistent dry cough is another hallmark symptom. Unlike other types of coughs, this one does not produce mucus and can be challenging to alleviate.
Fatigue
Many individuals with interstitial lung disease experience extreme tiredness and fatigue, which can interfere with daily activities.
Weight Loss
Unexplained weight loss is sometimes observed in people with advanced stages of the disease.
Clubbing of Fingers
In some cases, the fingertips may become enlarged or rounded, a condition known as clubbing. This occurs due to low oxygen levels in the blood.
Diagnosis of Interstitial Lung Disease
Diagnosing interstitial lung disease requires a comprehensive approach, as its symptoms can mimic those of other respiratory conditions. Healthcare providers typically use a combination of methods to confirm the diagnosis.
Medical History and Physical Examination
The first step involves taking a detailed medical history and conducting a thorough physical examination. Doctors will ask about symptoms, exposure to potential irritants, and any family history of lung disease.
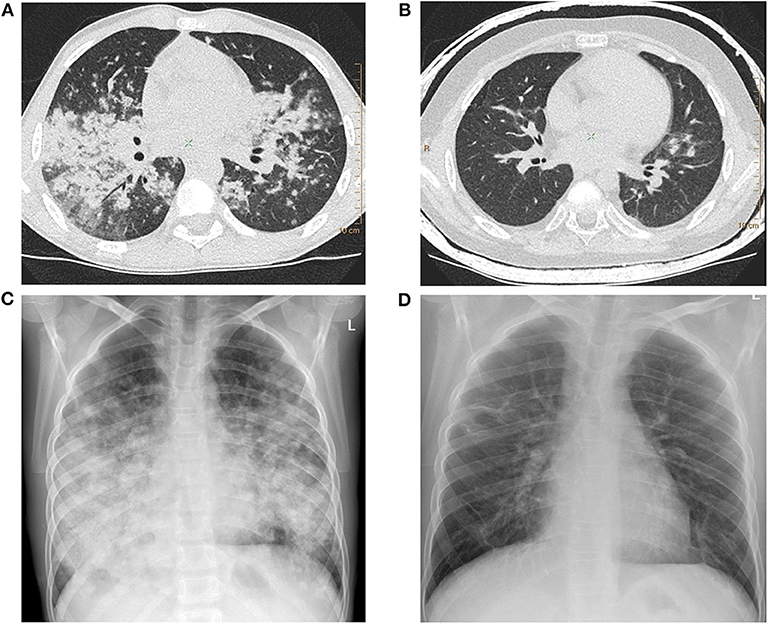
Imaging Tests
Imaging tests play a critical role in diagnosing interstitial lung disease. These include:
- Chest X-rays: Provide initial images of the lungs to identify abnormalities.
- High-Resolution CT Scans: Offer detailed pictures of the lung tissue, helping to pinpoint areas of scarring or inflammation.
Pulmonary Function Tests
Pulmonary function tests measure how well the lungs are working. These tests assess lung capacity, airflow, and the efficiency of oxygen transfer into the bloodstream.
Biopsy
In some cases, a biopsy may be necessary to obtain a small sample of lung tissue for analysis. This procedure helps determine the specific type of interstitial lung disease and guides treatment decisions.
Blood Tests
Blood tests can help rule out other conditions and detect markers of inflammation or autoimmune disorders that may be contributing to the disease.
Treatment and Care for Interstitial Lung Disease
While there is no cure for most forms of interstitial lung disease, various treatments can help manage symptoms, slow disease progression, and improve quality of life.
Medications
Several medications are used to address inflammation and slow the progression of scarring in the lungs. These include:
- Corticosteroids: Reduce inflammation in the lungs.
- Immunosuppressants: Suppress the immune system to prevent further damage.
- Antifibrotic Drugs: Slow the formation of scar tissue in certain types of the disease.
Oxygen Therapy
For individuals with low oxygen levels, supplemental oxygen therapy can help ease breathing and improve overall comfort. Portable oxygen devices allow patients to maintain an active lifestyle while receiving the support they need.
Pulmonary Rehabilitation
Pulmonary rehabilitation programs combine exercise, education, and counseling to help individuals manage their condition. These programs focus on improving endurance, teaching breathing techniques, and providing emotional support.
Lifestyle Modifications
Making certain lifestyle changes can also play a significant role in managing interstitial lung disease:
- Quitting smoking to reduce further lung damage.
- Avoiding exposure to pollutants and irritants.
- Eating a balanced diet to maintain strength and energy.
- Staying physically active within safe limits.
Lung Transplantation
In severe cases where other treatments have failed, a lung transplant may be considered. This option is typically reserved for younger patients with no other major health issues.
Emotional and Psychological Support
Living with interstitial lung disease can take a toll on mental health. Many individuals experience anxiety, depression, or feelings of isolation due to the challenges of managing a chronic illness. Seeking emotional and psychological support through counseling, support groups, or therapy can be invaluable in coping with the emotional aspects of the disease.
Prevention Strategies
While not all cases of interstitial lung disease can be prevented, certain measures can reduce the risk of developing the condition:
- Wearing protective gear when exposed to harmful substances at work.
- Avoiding smoking and secondhand smoke.
- Addressing underlying health conditions promptly.
- Regular check-ups with a healthcare provider to monitor lung health.
Research and Advances in Treatment
Ongoing research continues to shed light on the mechanisms behind interstitial lung disease and explore new treatment options. Scientists are investigating the role of genetics, stem cell therapy, and targeted medications to improve outcomes for patients. Staying informed about advancements in the field can empower individuals and their families to make educated decisions about care.