Inflammatory Bowel Disease, commonly abbreviated as IBD, is a group of chronic conditions that cause inflammation in the digestive tract. This condition significantly impacts the quality of life for millions of people worldwide. It primarily includes two main types: Crohn’s disease and ulcerative colitis. Both conditions share some similarities but also have distinct characteristics. Understanding the types, causes, symptoms, and treatments of this condition is crucial for patients, caregivers, and healthcare providers alike. In this article, we will delve into these aspects to provide a comprehensive overview.
Types of Inflammatory Bowel Disease
Crohn’s Disease
Crohn’s disease is one of the two primary forms of inflammatory bowel disease. It can affect any part of the gastrointestinal tract, from the mouth to the anus, but it most commonly occurs in the small intestine and the beginning of the large intestine. The inflammation caused by this condition often spreads deep into the layers of the affected tissue, leading to complications such as strictures, fistulas, and abscesses.
- Characteristics: Patchy areas of inflammation, with healthy tissue interspersed between affected regions.
- Common Sites: Terminal ileum (end of the small intestine) and colon.
- Potential Complications: Bowel obstruction, malnutrition, and increased risk of colorectal cancer.
Ulcerative Colitis
Unlike Crohn’s disease, ulcerative colitis only affects the colon and rectum. The inflammation typically begins in the rectum and may extend continuously to other parts of the colon. The innermost lining of the colon becomes inflamed and develops ulcers, which produce pus and mucus. This leads to frequent and urgent bowel movements, often accompanied by blood or pus.
- Characteristics: Continuous inflammation limited to the colon and rectum.
- Common Sites: Rectum and sigmoid colon, though it can involve the entire colon.
- Potential Complications: Severe bleeding, toxic megacolon, and an increased risk of colorectal cancer.
Causes of Inflammatory Bowel Disease
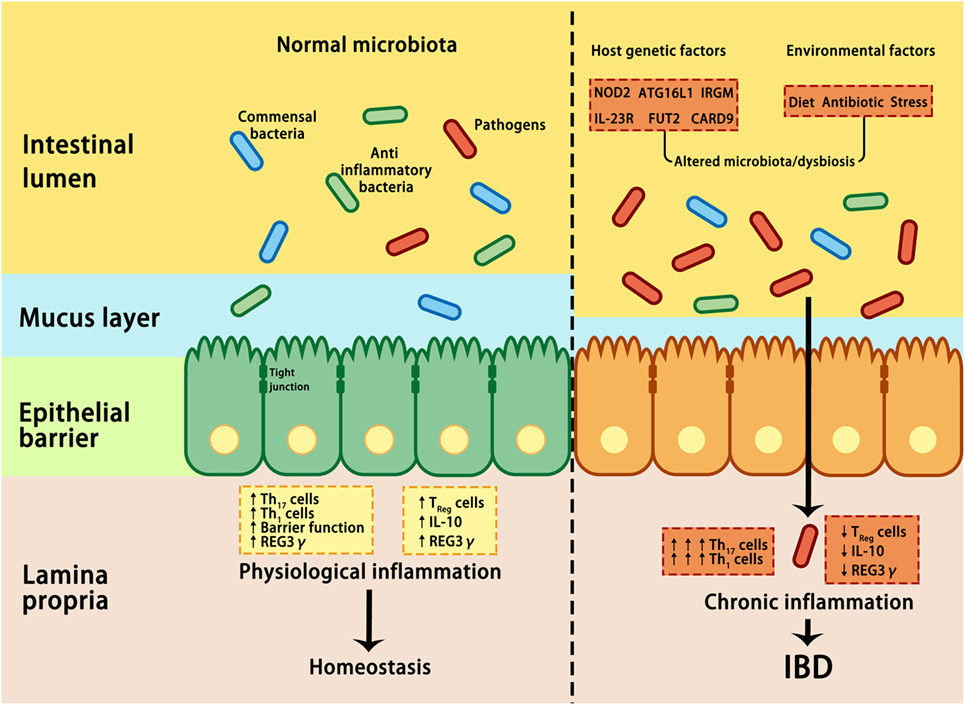
The exact cause of inflammatory bowel disease remains unknown, but researchers believe that it results from a combination of genetic, environmental, and immune system factors. Below are some key contributors:
Genetic Factors
Studies suggest that individuals with a family history of inflammatory bowel disease are at a higher risk of developing the condition. Certain genes have been identified as potential markers for susceptibility. However, having these genes does not guarantee that a person will develop the disease, indicating that other factors also play a role.
Immune System Dysfunction
Inflammatory bowel disease is believed to result from an abnormal immune response. Normally, the immune system defends the body against harmful invaders like bacteria and viruses. However, in individuals with this condition, the immune system mistakenly attacks the cells in the digestive tract, causing inflammation. This autoimmune reaction may be triggered by an environmental factor, such as a virus or bacterium.
Environmental Triggers
Several environmental factors have been linked to the development of inflammatory bowel disease. These include:
- Diet: A diet high in fat or refined foods may increase the risk.
- Smoking: Smoking is a known risk factor for Crohn’s disease but appears to offer some protection against ulcerative colitis.
- Medications: Nonsteroidal anti-inflammatory drugs, antibiotics, and oral contraceptives may contribute to the onset of the disease.
- Geography: The condition is more common in industrialized countries, suggesting that urbanization and modern lifestyles may play a role.
Symptoms of Inflammatory Bowel Disease
The symptoms of inflammatory bowel disease vary depending on the type and severity of the condition. Some individuals experience mild symptoms, while others face severe and debilitating effects. Below are the most common symptoms associated with both Crohn’s disease and ulcerative colitis.
Gastrointestinal Symptoms
- Diarrhea: Frequent loose stools, sometimes accompanied by blood or mucus.
- Abdominal Pain: Cramping and discomfort, often localized to the lower abdomen.
- Rectal Bleeding: Blood in the stool, more common in ulcerative colitis.
- Urgency to Defecate: A sudden and uncontrollable need to use the bathroom.
- Tenesmus: A feeling of incomplete bowel evacuation.
Systemic Symptoms
In addition to gastrointestinal issues, inflammatory bowel disease can cause systemic symptoms that affect the entire body. These include:
- Fatigue: Persistent tiredness due to chronic inflammation and nutrient deficiencies.
- Fever: Low-grade fevers are common during flare-ups.
- Weight Loss: Unintentional weight loss due to reduced appetite and malabsorption of nutrients.
- Nutritional Deficiencies: Anemia, vitamin D deficiency, and other imbalances are common.
Extraintestinal Manifestations
Inflammatory bowel disease can also affect organs outside the digestive tract. These extraintestinal manifestations include:
- Joint Pain: Arthritis or joint inflammation, particularly in larger joints like knees and hips.
- Skin Conditions: Erythema nodosum (painful red bumps) and pyoderma gangrenosum (skin ulcers).
- Eye Disorders: Uveitis (eye inflammation) and episcleritis (redness and irritation).
- Liver Problems: Primary sclerosing cholangitis, a condition affecting bile ducts.
Treatments for Inflammatory Bowel Disease
While there is currently no cure for inflammatory bowel disease, various treatments aim to reduce inflammation, manage symptoms, and achieve long-term remission. The treatment plan depends on the type and severity of the condition, as well as the patient’s overall health. Below are the primary approaches to managing inflammatory bowel disease.
Medications
Medications are the cornerstone of treatment for inflammatory bowel disease. They help control inflammation and prevent flare-ups. Commonly prescribed medications include:
- Aminosalicylates: Anti-inflammatory drugs like sulfasalazine and mesalamine, often used for mild to moderate cases of ulcerative colitis.
- Corticosteroids: Powerful anti-inflammatory medications like prednisone, used for short-term relief during severe flare-ups.
- Immunomodulators: Drugs like azathioprine and methotrexate, which suppress the immune system to reduce inflammation.
- Biologics: Advanced therapies like infliximab and adalimumab, which target specific proteins involved in the inflammatory process.
Dietary and Lifestyle Changes
Diet and lifestyle modifications can significantly improve symptoms and overall well-being. While no single diet works for everyone, the following strategies are commonly recommended:
- Low-Fiber Diet: Reducing fiber intake during flare-ups to minimize irritation in the digestive tract.
- Hydration: Staying well-hydrated to counteract the effects of diarrhea and fluid loss.
- Smoking Cessation: Quitting smoking is crucial for individuals with Crohn’s disease.
- Stress Management: Techniques like yoga, meditation, and therapy can help reduce stress, which may trigger flare-ups.
Surgery
In cases where medications and lifestyle changes are insufficient, surgery may be necessary. Surgical options differ based on the type of inflammatory bowel disease:
- Crohn’s Disease: Surgery may involve removing damaged portions of the digestive tract or repairing complications like fistulas and strictures.
- Ulcerative Colitis: A colectomy, or removal of the colon, may be performed in severe cases. This procedure often eliminates the disease entirely.
Emerging Therapies
Research into new treatments for inflammatory bowel disease is ongoing. Some promising areas include:
- Stem Cell Therapy: Using stem cells to regenerate damaged tissues in the digestive tract.
- Microbiome Modulation: Manipulating gut bacteria to restore balance and reduce inflammation.
- Personalized Medicine: Tailoring treatments based on an individual’s genetic profile and disease characteristics.
These advancements hold the potential to revolutionize the management of inflammatory bowel disease in the future.