Inflammatory conditions affecting the gastrointestinal tract can significantly impact an individual’s quality of life. Among these conditions, inflammation of the rectum, commonly referred to as proctitis, is a medical concern that requires attention due to its potential complications. Proctitis can arise from various causes, present with distinct symptoms, and necessitate specific treatment approaches. This article delves into the intricacies of this condition, shedding light on its origins, manifestations, and management strategies.

What Is Inflammation of the Rectum?
Inflammation of the rectum occurs when the lining of the rectum becomes irritated or swollen. The rectum is the final section of the large intestine, connecting the colon to the anus. Its primary function is to store stool until it is expelled from the body. When the rectal lining becomes inflamed, it can lead to discomfort, pain, and other distressing symptoms. This condition is often associated with inflammatory bowel diseases, infections, or other underlying health issues.
Common Causes of Rectal Inflammation
The causes of inflammation in the rectum are diverse and can be broadly categorized into several groups:
Infections
- Bacterial Infections: Certain bacteria, such as those causing sexually transmitted infections like gonorrhea or chlamydia, can lead to inflammation of the rectum. These infections are more common in individuals who engage in anal intercourse.
- Viral Infections: Viruses such as herpes simplex or cytomegalovirus can also cause inflammation. These infections may occur in individuals with weakened immune systems, such as those living with human immunodeficiency virus.
- Fungal Infections: Although less common, fungal infections like candidiasis can sometimes result in rectal inflammation, particularly in individuals with diabetes or those taking antibiotics for extended periods.
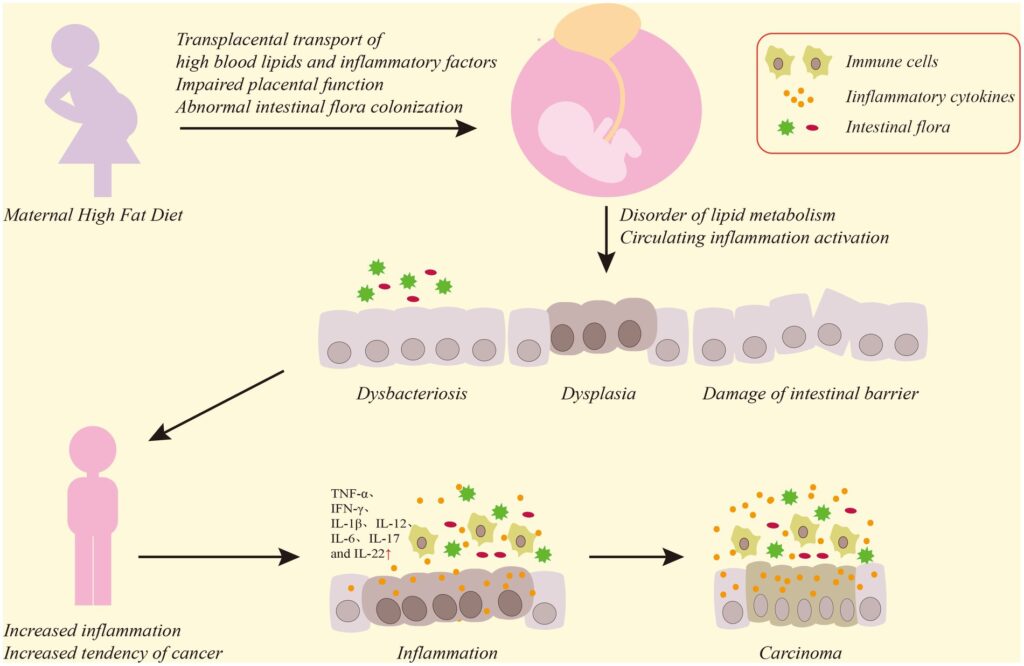
Inflammatory Bowel Diseases
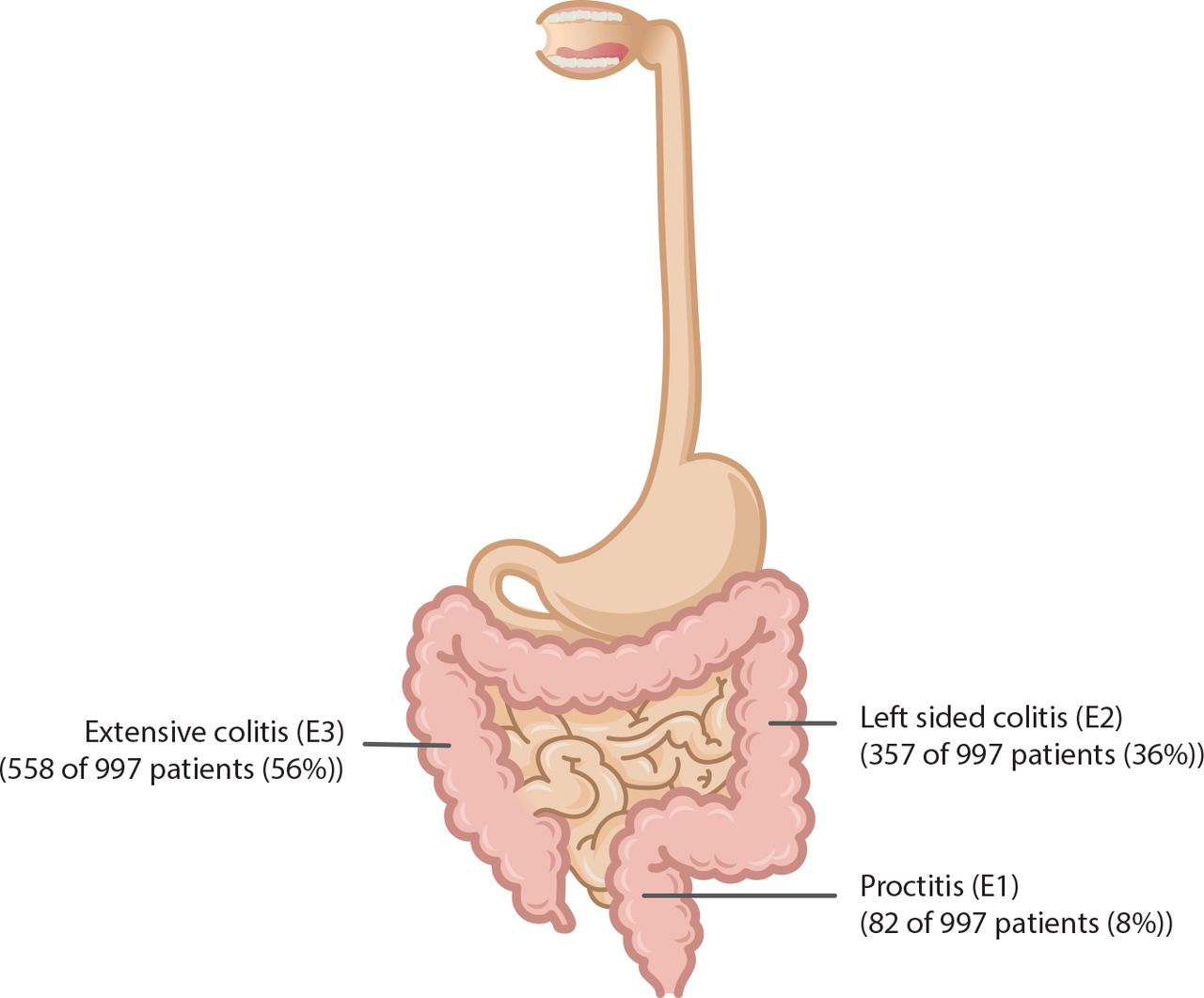
- Ulcerative Colitis: This chronic condition causes inflammation and ulcers in the lining of the large intestine and rectum. It is one of the most common causes of inflammation of the rectum.
- Crohn’s Disease: While Crohn’s disease primarily affects the small intestine, it can also involve the rectum and cause inflammation in this area.
Radiation Therapy
Radiation therapy used to treat cancers in the pelvic region, such as prostate or cervical cancer, can damage the rectal lining and lead to inflammation. This condition, known as radiation proctitis, may develop during or after treatment.
Trauma or Injury
Physical trauma to the rectum, such as from the insertion of foreign objects or aggressive medical procedures, can irritate the lining and trigger inflammation. Additionally, excessive use of enemas or laxatives may contribute to this condition.
Allergic Reactions
In rare cases, allergic reactions to certain foods or substances can cause inflammation in the rectum. This type of reaction is more common in individuals with food sensitivities or allergies.
Symptoms of Rectal Inflammation
The symptoms of inflammation of the rectum can vary depending on the underlying cause and severity of the condition. Common signs and symptoms include:
- Rectal Pain: Individuals often experience discomfort or pain in the rectal area, which may worsen during bowel movements.
- Bleeding: Blood in the stool or on toilet paper after wiping is a frequent symptom. The blood may appear bright red, indicating that it originates from the lower part of the digestive tract.
- Diarrhea: Persistent diarrhea or loose stools can occur, sometimes accompanied by mucus discharge.
- Tenesmus: A constant urge to have a bowel movement, even when the rectum is empty, is a hallmark symptom of rectal inflammation.
- Pain During Bowel Movements: Passing stool may become painful, leading to reluctance or fear of defecation.
- Fever and Fatigue: In cases where infection is the cause, systemic symptoms such as fever and fatigue may accompany rectal inflammation.
How Is Rectal Inflammation Diagnosed?
Diagnosing inflammation of the rectum typically involves a combination of clinical evaluation, laboratory tests, and imaging studies. Healthcare providers may use the following methods to identify the condition:
Medical History and Physical Examination
A detailed medical history helps healthcare providers understand the duration, severity, and possible triggers of symptoms. During a physical examination, a digital rectal exam may be performed to assess the rectal lining for tenderness, swelling, or other abnormalities.
Endoscopic Procedures
- Proctoscopy: This procedure involves inserting a thin, flexible tube with a camera into the rectum to visualize the lining and identify areas of inflammation or ulcers.
- Sigmoidoscopy or Colonoscopy: These procedures allow for a more comprehensive examination of the rectum and colon, helping to rule out other conditions like ulcerative colitis or Crohn’s disease.
Laboratory Tests
- Stool Tests: Analyzing a stool sample can help detect infections, blood, or inflammatory markers.
- Blood Tests: Blood work may reveal elevated white blood cell counts or markers of inflammation, such as C-reactive protein.
Imaging Studies
In some cases, imaging techniques like magnetic resonance imaging or computed tomography scans may be used to evaluate the extent of inflammation or identify complications.
Treatment Options for Rectal Inflammation
The treatment of inflammation of the rectum depends on its underlying cause and severity. A multidisciplinary approach is often necessary to manage symptoms effectively and prevent recurrence. Below are some common treatment strategies:
Medications
- Antibiotics: If a bacterial infection is the cause, antibiotics may be prescribed to eliminate the infection and reduce inflammation.
- Antiviral Medications: For viral infections, antiviral drugs can help control the infection and alleviate symptoms.
- Anti-inflammatory Drugs: Nonsteroidal anti-inflammatory drugs or corticosteroids may be used to reduce inflammation and provide relief from pain.
- Immunosuppressants: In cases of inflammatory bowel diseases, medications that suppress the immune system may be required to manage chronic inflammation.
Dietary and Lifestyle Modifications
Making changes to diet and lifestyle can play a crucial role in managing rectal inflammation:
- High-Fiber Diet: Consuming fiber-rich foods can help regulate bowel movements and reduce irritation in the rectum.
- Avoiding Irritants: Spicy foods, alcohol, and caffeine may exacerbate symptoms and should be avoided.
- Hydration: Staying well-hydrated supports digestive health and prevents constipation, which can worsen inflammation.
Topical Treatments
Topical medications, such as suppositories or enemas containing corticosteroids or anti-inflammatory agents, can deliver targeted relief to the inflamed rectal lining.
Radiation Proctitis Management
For individuals with radiation-induced rectal inflammation, treatments may include:
- Hyperbaric Oxygen Therapy: This therapy involves breathing pure oxygen in a pressurized chamber to promote healing of damaged tissues.
- Sucralfate Enemas: Sucralfate, a medication that forms a protective barrier over the inflamed tissue, can be administered via enema to reduce symptoms.
Surgical Interventions
In severe cases where conservative treatments fail, surgical options may be considered. These include procedures to remove damaged tissue or repair structural abnormalities contributing to inflammation.
Preventing Recurrence of Rectal Inflammation
While not all cases of rectal inflammation can be prevented, certain measures can reduce the risk of recurrence:
- Safe Sexual Practices: Using protection during sexual activity can prevent infections that may lead to inflammation.
- Regular Medical Checkups: Monitoring for early signs of inflammatory bowel diseases or other conditions can facilitate timely intervention.
- Managing Underlying Conditions: Properly managing conditions like diabetes or autoimmune disorders can minimize the risk of complications.
Living with Rectal Inflammation
Living with inflammation of the rectum can be challenging, but with appropriate care and support, individuals can manage their symptoms effectively. Open communication with healthcare providers, adherence to treatment plans, and lifestyle adjustments are essential components of long-term management. Support groups and counseling may also provide emotional relief and practical advice for coping with the condition.