Myocarditis, also known as inflammation of the heart muscle, is a condition that can affect individuals of all ages. While it may not always present obvious symptoms, myocarditis can have serious consequences if left untreated. This article explores the causes, symptoms, and treatments of this condition to provide a comprehensive understanding of how it impacts the body and what can be done to manage it effectively.
Understanding Myocarditis
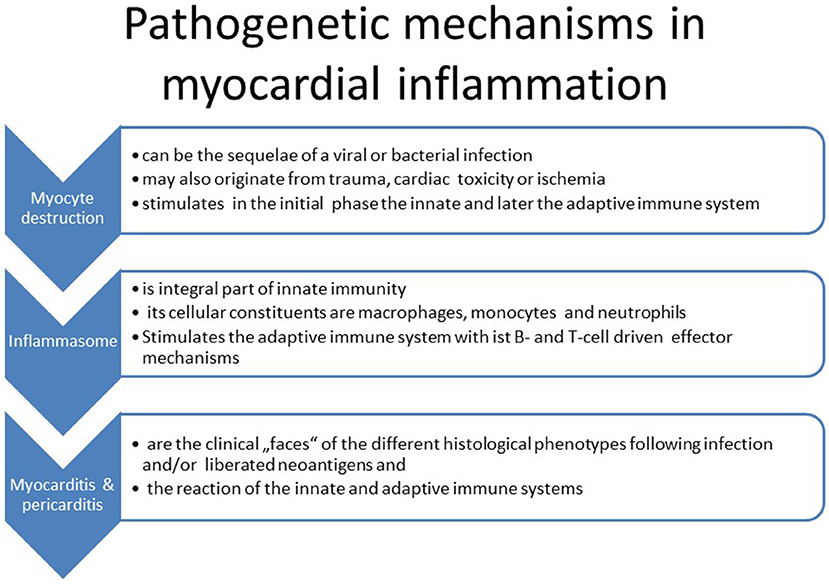
The heart is a vital organ responsible for pumping blood throughout the body, delivering oxygen and nutrients to tissues. The muscular layer of the heart, called the myocardium, plays a crucial role in this process. When the myocardium becomes inflamed due to infection, autoimmune disorders, or other factors, it can impair the heart’s ability to function properly. This condition is referred to as myocarditis.
While myocarditis is often mild and resolves on its own, severe cases can lead to complications such as heart failure, arrhythmias, or even sudden cardiac death. Understanding the underlying causes, recognizing the symptoms, and seeking timely treatment are essential steps in managing this condition.
Causes of Myocarditis
There are several potential causes of inflammation in the heart muscle. These causes can vary widely depending on individual health conditions, environmental factors, and exposure to pathogens. Below are some of the most common causes:
Viral Infections
- Coxsackievirus: This virus is one of the leading causes of viral myocarditis, particularly in children and young adults.
- Influenza: The flu virus can sometimes lead to inflammation of the heart muscle, especially in cases of severe infection.
- Epstein-Barr Virus: Known for causing mononucleosis, this virus has also been linked to myocarditis.
- Adenovirus: Commonly associated with respiratory infections, adenoviruses can occasionally affect the heart.
Bacterial Infections
- Diphtheria: A bacterial infection that can damage the heart muscle if left untreated.
- Lyme Disease: Caused by tick bites, Lyme disease can lead to inflammation of the heart in some cases.
- Staphylococcus and Streptococcus: These bacteria can cause infections that spread to the heart tissue.
Autoimmune Disorders
In some cases, the immune system mistakenly attacks the heart muscle, leading to inflammation. Conditions such as lupus, rheumatoid arthritis, and scleroderma are examples of autoimmune disorders that can increase the risk of myocarditis.
Medications and Toxins
Certain medications and exposure to toxins can also trigger inflammation of the heart muscle. Examples include:
- Antibiotics like penicillin
- Chemotherapy drugs
- Excessive alcohol consumption
- Illicit drug use, such as cocaine
Other Causes
Less common causes of myocarditis include fungal infections, parasitic infections, and radiation therapy for cancer treatment. Additionally, physical trauma or extreme stress on the body can sometimes lead to inflammation of the heart muscle.
Symptoms of Myocarditis
The symptoms of inflammation of the heart muscle can vary significantly from person to person. Some individuals may experience no symptoms at all, while others may develop severe complications. Common signs and symptoms include:
Mild Symptoms
- Fatigue or weakness
- Shortness of breath, especially during physical activity
- Mild chest pain or discomfort
- Swelling in the legs, ankles, or feet
Severe Symptoms
- Rapid or irregular heartbeat
- Sharp, stabbing chest pain
- Fainting or dizziness
- Difficulty breathing, even at rest
Symptoms in Children
In children, myocarditis may present differently than in adults. Parents should watch for signs such as:
- Fever
- Poor feeding or appetite
- Irritability or lethargy
- Rapid breathing or difficulty breathing
It is important to note that many of these symptoms can mimic those of other conditions, such as the flu or a common cold. For this reason, it is crucial to consult a healthcare professional if any of these symptoms persist or worsen over time.
Diagnosing Myocarditis
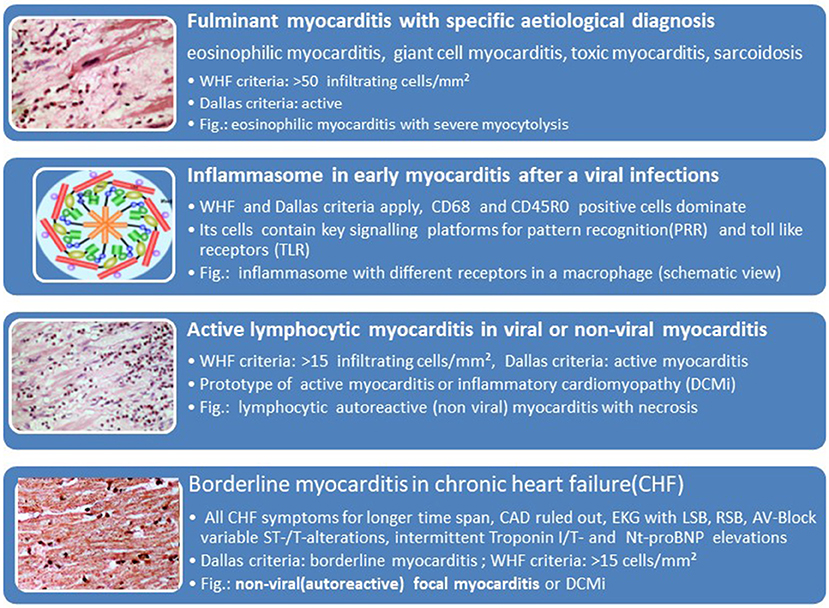
Diagnosing inflammation of the heart muscle can be challenging because its symptoms often overlap with those of other conditions. Healthcare providers typically use a combination of methods to confirm a diagnosis:
Medical History and Physical Examination
A thorough review of the patient’s medical history and a physical examination are the first steps in diagnosing myocarditis. The doctor will ask about recent illnesses, exposure to infections, and any medications or substances the patient may have used.
Diagnostic Tests
- Electrocardiogram (ECG): This test measures the electrical activity of the heart and can detect abnormal rhythms or signs of heart damage.
- Echocardiogram: An ultrasound of the heart that provides images of its structure and function, helping to identify areas of inflammation or reduced pumping ability.
- Blood Tests: Blood samples can reveal elevated levels of certain enzymes or markers that indicate heart muscle damage.
- Magnetic Resonance Imaging (MRI): This imaging technique provides detailed pictures of the heart and can help identify areas of inflammation.
- Endomyocardial Biopsy: In rare cases, a small sample of heart tissue may be taken for analysis to confirm the presence of inflammation.
Treatment Options for Myocarditis
Treatment for inflammation of the heart muscle depends on the severity of the condition and its underlying cause. In mild cases, the condition may resolve on its own with rest and supportive care. However, more severe cases require targeted interventions to prevent complications.
Rest and Lifestyle Modifications
For patients with mild myocarditis, doctors often recommend:
- Avoiding strenuous physical activity to reduce strain on the heart
- Limiting salt intake to reduce fluid retention
- Quitting smoking and avoiding alcohol or recreational drugs
Medications
Depending on the specific needs of the patient, medications may be prescribed to manage symptoms and support heart function:
- Anti-inflammatory Drugs: Medications such as ibuprofen or corticosteroids may be used to reduce inflammation.
- Heart Failure Medications: Drugs like beta-blockers or ACE inhibitors can help improve heart function and reduce the workload on the heart.
- Antibiotics or Antiviral Drugs: If the condition is caused by a bacterial or viral infection, appropriate medications may be prescribed to treat the underlying cause.
Hospitalization and Advanced Treatments
In severe cases, hospitalization may be necessary to monitor and treat complications. Advanced treatments may include:
- Intravenous Medications: Administered to stabilize heart function and address complications such as arrhythmias.
- Ventricular Assist Devices: Mechanical devices that help the heart pump blood in cases of severe heart failure.
- Heart Transplant: In rare instances where the heart is severely damaged, a transplant may be considered as a last resort.
Addressing Underlying Conditions
If myocarditis is caused by an autoimmune disorder or exposure to toxins, treating the underlying condition is essential. This may involve immunosuppressive therapy, lifestyle changes, or discontinuing harmful medications.
Preventing Myocarditis
While not all cases of inflammation of the heart muscle can be prevented, certain measures can reduce the risk of developing the condition:
- Practicing good hygiene to avoid viral and bacterial infections
- Staying up-to-date with vaccinations, including those for influenza and other preventable diseases
- Avoiding excessive alcohol consumption and illicit drug use
- Managing chronic conditions such as diabetes or autoimmune disorders
When to Seek Medical Attention
Individuals experiencing symptoms such as chest pain, shortness of breath, or fainting should seek immediate medical attention. Early diagnosis and treatment can significantly improve outcomes and reduce the risk of complications.