Iliotibial Band Syndrome, commonly referred to as ITBS, is a prevalent condition that affects many individuals, particularly those who engage in activities like running, cycling, or hiking. This syndrome occurs when the iliotibial band, a thick band of connective tissue that runs along the outside of the thigh from the hip to the knee, becomes inflamed or irritated. Understanding the underlying causes, recognizing the symptoms, and exploring effective treatments are essential for managing this condition and preventing its recurrence.
What Is the Iliotibial Band?
The iliotibial band is a dense strip of fibrous tissue that extends from the pelvis to just below the knee. Its primary function is to stabilize the knee joint during movement and assist with leg motion. It works closely with muscles such as the glutes and tensor fasciae latae to ensure smooth and efficient movement. However, repetitive stress or improper use can lead to irritation and inflammation, resulting in discomfort and pain.
Common Causes of Iliotibial Band Syndrome
Several factors contribute to the development of this condition. Identifying these causes can help individuals take preventive measures and address the root of the problem.
Overuse and Repetitive Motion
One of the most common causes of this condition is overuse. Activities that involve repetitive bending and straightening of the knee, such as running or cycling, place constant stress on the iliotibial band. Over time, this repetitive motion can cause friction between the band and the bony structures of the knee, leading to inflammation.
Poor Biomechanics
- Improper Footwear: Wearing shoes that do not provide adequate support or cushioning can alter the way the foot strikes the ground, affecting the alignment of the entire leg.
- Leg Length Discrepancy: A difference in the length of the legs can cause uneven distribution of weight and pressure, increasing stress on the iliotibial band.
- Muscle Imbalances: Weakness or tightness in the muscles surrounding the hips, thighs, and knees can disrupt the natural movement patterns, placing additional strain on the band.
Inadequate Warm-Up or Stretching
Failing to warm up properly before physical activity or neglecting to stretch afterward can leave the muscles and connective tissues stiff and more prone to injury. The iliotibial band, being a relatively inflexible structure, is particularly vulnerable to damage without proper preparation.
Terrain and Training Errors
Running or exercising on uneven surfaces, such as hills or slanted roads, can exacerbate stress on the iliotibial band. Additionally, increasing the intensity or duration of workouts too quickly can overwhelm the body’s ability to adapt, leading to overuse injuries.
Symptoms of Iliotibial Band Syndrome
Recognizing the symptoms early can prevent the condition from worsening and allow for timely intervention. The following signs are commonly associated with this condition:
Pain on the Outer Knee
The hallmark symptom is a sharp or burning pain located on the outer side of the knee. This discomfort typically worsens during activities that involve repetitive knee bending, such as running, walking downhill, or climbing stairs. In some cases, the pain may radiate upward toward the hip or downward along the shin.
Swelling and Tenderness
Inflammation of the iliotibial band can cause localized swelling around the knee area. The affected region may also feel tender to the touch, making it uncomfortable to apply pressure or kneel.
Popping or Snapping Sensation
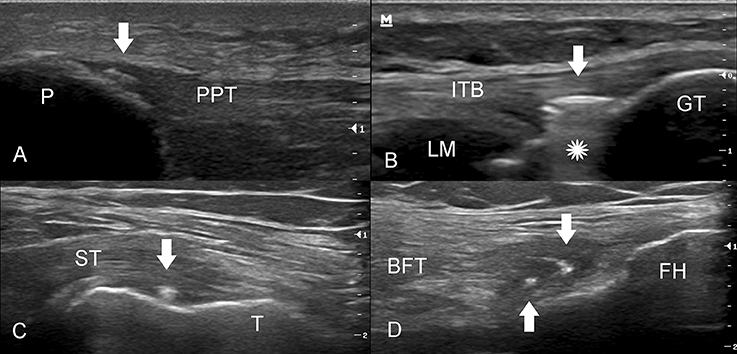
Some individuals report hearing or feeling a popping or snapping sound near the knee during movement. This sensation occurs when the band rubs against the bony prominence of the femur, creating friction and irritation.
Stiffness and Reduced Mobility
As the condition progresses, stiffness in the knee joint may develop, limiting the range of motion. Activities that were once easy, such as squatting or bending, may become challenging due to discomfort and restricted movement.
Treatment Options for Iliotibial Band Syndrome
Managing this condition involves a combination of rest, physical therapy, and lifestyle adjustments. The goal of treatment is to reduce inflammation, alleviate pain, and restore normal function.
Rest and Activity Modification
The first step in treating this condition is to rest the affected leg and avoid activities that aggravate the symptoms. Continuing to push through the pain can worsen the inflammation and prolong recovery. Instead, individuals should focus on low-impact exercises, such as swimming or yoga, which place minimal stress on the knees.
Ice Therapy
Applying ice packs to the painful area can help reduce swelling and numb the discomfort. Ice therapy is most effective when applied for 15 to 20 minutes at a time, several times a day, especially after physical activity.
Physical Therapy
A physical therapist can design a personalized rehabilitation program to address muscle imbalances and improve flexibility. Common exercises include:
- Stretching: Gentle stretches targeting the hips, thighs, and calves can help loosen tight muscles and relieve tension on the iliotibial band.
- Strengthening Exercises: Strengthening the gluteal muscles and core can enhance stability and reduce strain on the band.
- Foam Rolling: Using a foam roller to massage the outer thigh can break up adhesions and improve tissue mobility.
Orthotics and Proper Footwear
For individuals with biomechanical issues, custom orthotics or supportive footwear can correct alignment problems and distribute pressure more evenly across the foot and leg. Consulting a podiatrist or sports medicine specialist can help determine the appropriate interventions.
Medications
Over-the-counter nonsteroidal anti-inflammatory drugs, such as ibuprofen or naproxen, can help manage pain and reduce inflammation. However, these medications should be used sparingly and under the guidance of a healthcare professional to avoid potential side effects.
Corticosteroid Injections
In severe cases where conservative treatments fail to provide relief, a doctor may recommend corticosteroid injections to reduce inflammation in the affected area. While effective, this option is typically reserved for persistent or debilitating symptoms.
Surgical Intervention
Surgery is rarely necessary but may be considered if all other treatments have been exhausted and the condition continues to interfere with daily activities. The procedure typically involves releasing a portion of the iliotibial band to alleviate pressure and friction at the knee.
Preventive Measures to Avoid Recurrence
Once the symptoms have subsided, taking steps to prevent the condition from returning is crucial. Incorporating the following strategies into your routine can help maintain long-term health and mobility:
- Gradual Progression: Increase the intensity and duration of workouts gradually to allow the body to adapt without overloading the tissues.
- Cross-Training: Alternate high-impact activities with low-impact ones to minimize repetitive stress on the knees.
- Regular Stretching: Make stretching a regular part of your routine to maintain flexibility and prevent tightness in the muscles and connective tissues.
- Proper Technique: Ensure that you are using correct form and posture during exercise to reduce unnecessary strain on the body.
When to Seek Medical Attention
While many cases of this condition can be managed with self-care and conservative treatments, there are instances when medical attention is necessary. If the pain persists despite rest and home remedies, or if the symptoms worsen over time, it is important to consult a healthcare provider. Additionally, seek professional help if you experience significant swelling, redness, or warmth around the knee, as these could indicate a more serious underlying issue.