Idiopathic Intracranial Hypertension, often abbreviated as IIH, is a medical condition that affects the brain and its surrounding structures. This guide aims to provide a comprehensive overview of this condition, including its causes, symptoms, diagnosis, treatment options, and lifestyle considerations. Whether you are someone living with this condition or simply seeking to understand it better, this article will serve as a valuable resource.
Understanding Idiopathic Intracranial Hypertension
Idiopathic Intracranial Hypertension refers to a condition where there is increased pressure around the brain without any identifiable cause. The term “idiopathic” means that the exact reason for the elevated pressure remains unknown. This condition primarily affects women of childbearing age but can occur in individuals of all genders and ages.
What Happens in the Brain?
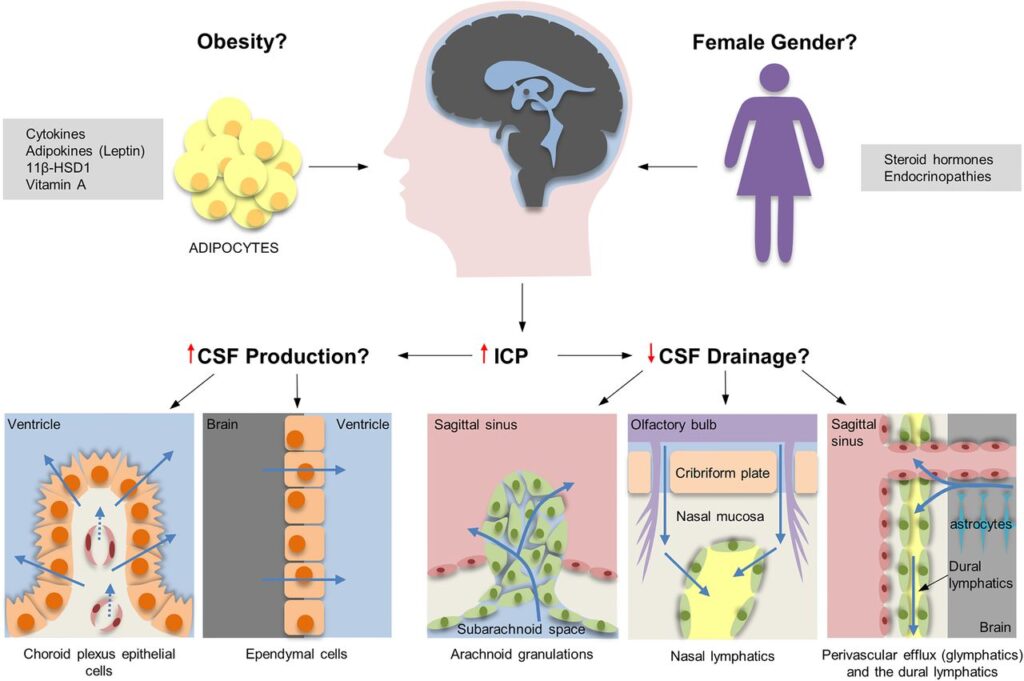
The brain and spinal cord are surrounded by a fluid called cerebrospinal fluid. This fluid acts as a cushion, protecting the brain from injury and helping it function properly. In cases of intracranial hypertension, the pressure of this fluid increases, leading to a range of symptoms. Unlike other forms of intracranial hypertension, which may result from tumors, infections, or blood clots, this condition occurs without any apparent underlying cause.
Symptoms to Watch For
Recognizing the symptoms of this condition is crucial for early diagnosis and treatment. Below are some of the most common signs:
- Severe Headaches: These headaches are often described as throbbing and can worsen over time. They may be accompanied by nausea or vomiting.
- Vision Problems: Blurred vision, double vision, or temporary loss of vision are common. Some individuals may also experience blind spots.
- Pulsatile Tinnitus: This refers to a whooshing or ringing sound in the ears that corresponds with the heartbeat.
- Pain Behind the Eyes: Individuals may feel discomfort or pain behind the eyes, especially when moving them.
- Nausea and Vomiting: These symptoms can occur alongside headaches and may be mistaken for migraines.
If you or someone you know experiences these symptoms, it is essential to seek medical attention promptly.
Causes and Risk Factors
While the exact cause of this condition remains unknown, researchers have identified several factors that may increase the risk of developing it:
Obesity
One of the most significant risk factors is obesity. Studies have shown a strong correlation between excess body weight and the development of this condition. Fat cells may contribute to hormonal changes that affect cerebrospinal fluid dynamics.
Hormonal Influences
Hormonal fluctuations, particularly those related to estrogen, may play a role. This could explain why the condition is more prevalent in women, especially during their reproductive years.
Medications
Certain medications, such as tetracycline antibiotics, steroids, and birth control pills, have been linked to an increased risk. If you are taking any of these medications and experience symptoms, consult your healthcare provider.
Other Factors
Other potential contributors include sleep apnea, kidney disease, and vitamin A toxicity. While these factors do not directly cause the condition, they may exacerbate it in susceptible individuals.
Diagnosing the Condition
Diagnosing this condition involves a combination of clinical evaluation, imaging tests, and specialized procedures. Below is an overview of the diagnostic process:
Medical History and Physical Examination
Your doctor will begin by reviewing your medical history and conducting a thorough physical examination. They will ask about your symptoms, their duration, and any factors that worsen or alleviate them.
Neurological Examination
A neurological exam assesses brain function, including vision, hearing, balance, and reflexes. Abnormal findings, such as vision loss or difficulty moving the eyes, may indicate increased intracranial pressure.
Imaging Tests
To rule out other potential causes of intracranial hypertension, your doctor may order imaging tests such as:
- Magnetic Resonance Imaging (MRI): This test provides detailed images of the brain and can help identify structural abnormalities.
- Computed Tomography (CT) Scan: A CT scan uses X-rays to create cross-sectional images of the brain.
Lumbar Puncture
A lumbar puncture, also known as a spinal tap, is a key diagnostic tool. During this procedure, a needle is inserted into the lower back to measure cerebrospinal fluid pressure. Elevated pressure confirms the diagnosis.
Treatment Options
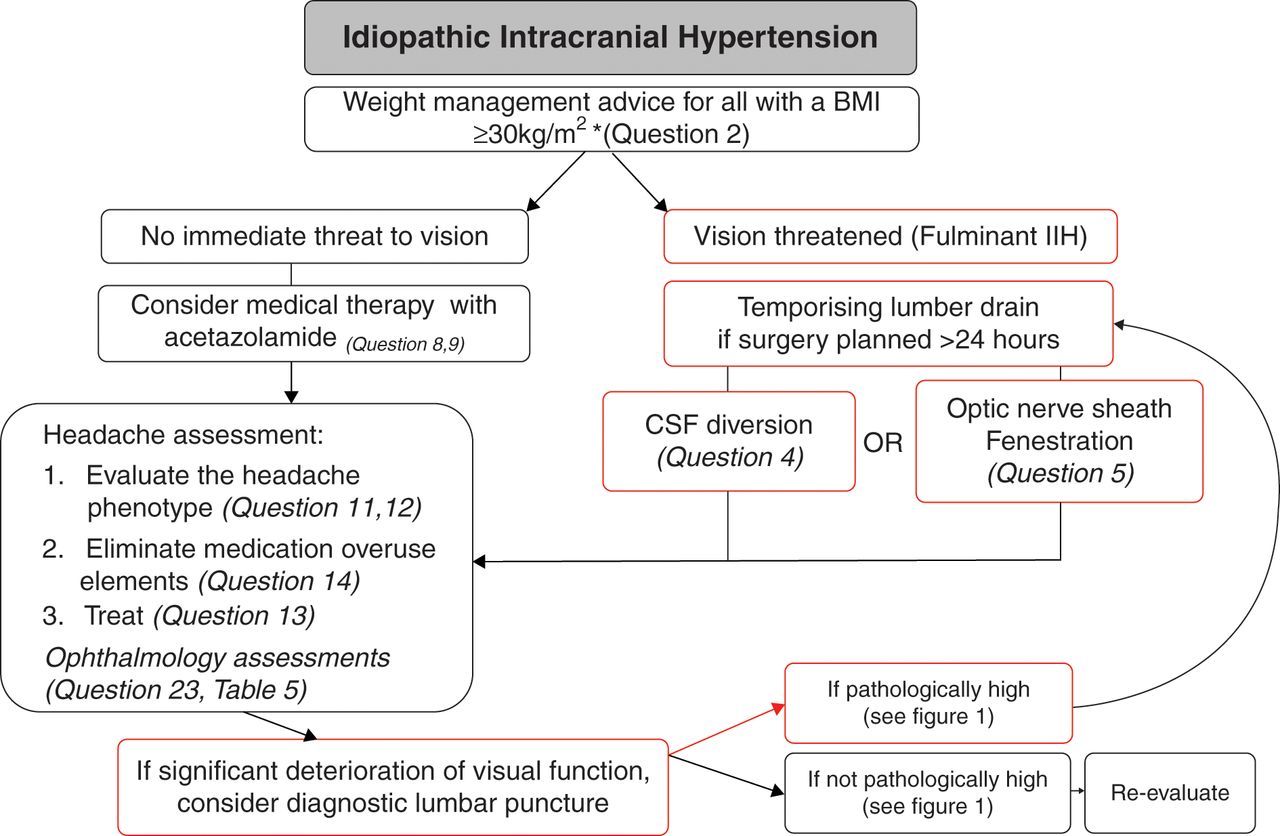
Treatment for this condition focuses on reducing intracranial pressure, alleviating symptoms, and preventing complications such as permanent vision loss. Below are the main approaches:
Weight Management
For individuals who are overweight or obese, losing weight is one of the most effective ways to manage the condition. Even modest weight loss can significantly reduce symptoms and improve outcomes.
Medications
Several medications can help lower intracranial pressure:
- Acetazolamide: This medication reduces the production of cerebrospinal fluid, thereby lowering pressure.
- Furosemide: A diuretic that helps eliminate excess fluid from the body.
- Pain Relievers: Over-the-counter or prescription pain medications can help manage headaches.
Surgical Interventions
In severe cases where medications and lifestyle changes are insufficient, surgery may be necessary. Common surgical options include:
- Optic Nerve Sheath Fenestration: This procedure relieves pressure on the optic nerve to prevent vision loss.
- Ventriculoperitoneal Shunt: A shunt is implanted to drain excess cerebrospinal fluid from the brain to the abdomen.
Lifestyle Considerations
Beyond medical treatments, certain lifestyle changes can help manage symptoms and improve quality of life:
Dietary Adjustments
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall health. Reducing sodium intake may also help manage fluid retention.
Regular Exercise
Engaging in regular physical activity can aid in weight management and improve cardiovascular health. Low-impact exercises such as walking, swimming, or yoga are excellent choices.
Stress Management
Chronic stress can exacerbate symptoms. Techniques such as meditation, deep breathing exercises, and mindfulness can help reduce stress levels.
Monitoring Vision
Regular eye exams are crucial for detecting and addressing vision changes early. Report any new or worsening symptoms to your healthcare provider immediately.
Living with the Condition
Living with this condition can be challenging, but with proper management, many individuals lead fulfilling lives. Building a strong support system, staying informed, and adhering to treatment plans are essential steps toward achieving optimal health.
Support Groups
Connecting with others who share similar experiences can provide emotional support and practical advice. Online forums and local support groups offer opportunities to engage with a community of individuals facing the same challenges.
Educating Yourself
Knowledge is empowering. Take the time to learn about the condition, its treatments, and strategies for managing symptoms. This will enable you to make informed decisions about your care.
Working with Healthcare Providers
Establishing a collaborative relationship with your healthcare team is vital. Be open about your symptoms, concerns, and goals, and work together to develop a personalized treatment plan.
Final Thoughts
While this condition can be daunting, understanding its intricacies and adopting proactive measures can make a significant difference. By staying vigilant about symptoms, adhering to treatment recommendations, and embracing healthy lifestyle habits, individuals can effectively manage this condition and minimize its impact on daily life.