Ichthyosis, often abbreviated as ICH, refers to a group of skin disorders characterized by dry, scaly, and sometimes thickened skin. These conditions can range from mild and manageable to severe and life-altering. While the term “ichthyosis” might sound unfamiliar to many, it affects countless individuals worldwide, making it crucial to understand its causes, symptoms, and treatment options. This guide will delve into the intricacies of ichthyosis, shedding light on its various forms, underlying mechanisms, and strategies for managing this challenging condition.
What is Ichthyosis?
Ichthyosis is derived from the Greek word “ichthys,” meaning fish, due to the resemblance of affected skin to fish scales. It encompasses a variety of genetic and acquired skin disorders that result in abnormal skin scaling and dryness. The condition can be present at birth or develop later in life, depending on its type and cause. While some forms are relatively mild and improve with age, others can significantly impact an individual’s quality of life.
Common Characteristics of Ichthyosis
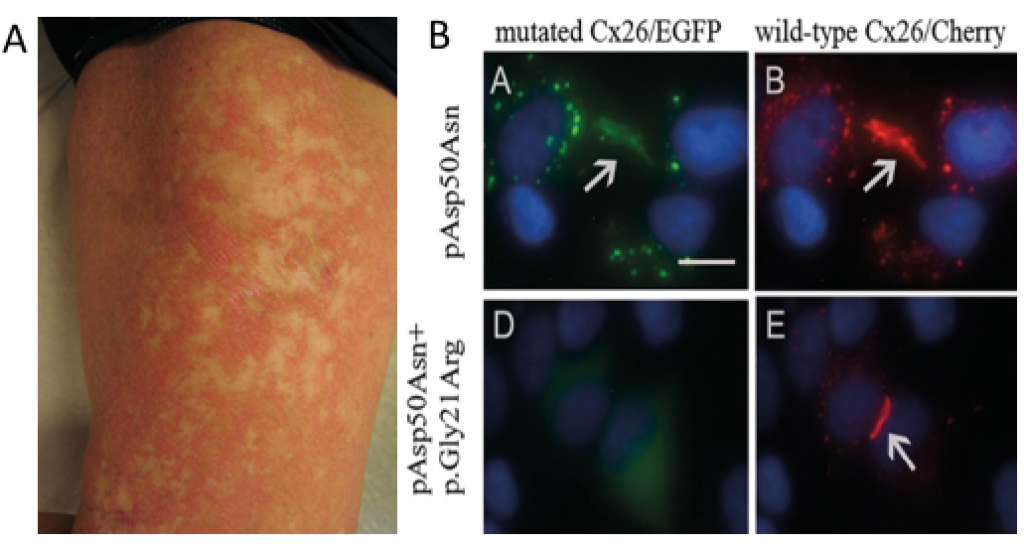
- Dry, rough, and scaly skin
- Thickened areas of skin, particularly on the arms and legs
- Flaking or peeling skin
- Cracks or fissures in the skin, which may lead to discomfort or infection
- In severe cases, restricted movement due to tight, thickened skin
Types of Ichthyosis
There are several types of ichthyosis, each with distinct features and underlying causes. Understanding these variations is essential for accurate diagnosis and appropriate treatment.
Ichthyosis Vulgaris
Ichthyosis Vulgaris is the most common form of ichthyosis, affecting approximately 1 in every 250 people. It is typically inherited in an autosomal dominant pattern, meaning only one parent needs to carry the gene for the condition to manifest. Symptoms usually appear in early childhood and include dry, scaly skin, particularly on the legs and lower arms. The severity of the condition can vary, with some individuals experiencing only mild dryness while others face more pronounced scaling.
X-Linked Ichthyosis
X-Linked Ichthyosis primarily affects males and is caused by a deficiency in the enzyme steroid sulfatase. This enzyme plays a crucial role in breaking down cholesterol sulfate in the skin. Without sufficient levels of this enzyme, the skin accumulates excess cholesterol sulfate, leading to thick, dark scales, especially on the neck, trunk, and lower extremities. Unlike Ichthyosis Vulgaris, X-Linked Ichthyosis tends to persist throughout life and does not improve with age.
Lamellar Ichthyosis
Lamellar Ichthyosis is a rare and more severe form of ichthyosis that is present at birth. Infants with this condition are often born encased in a collodion membrane, a shiny, tight layer of skin that sheds within the first few weeks of life. After shedding, the skin becomes covered in large, plate-like scales. Lamellar Ichthyosis can also cause complications such as overheating, dehydration, and increased susceptibility to infections due to impaired skin barrier function.
Epidermolytic Ichthyosis
Epidermolytic Ichthyosis, formerly known as Epidermolytic Hyperkeratosis, is another rare genetic disorder that results in fragile, blistering skin at birth. As the child grows, the skin develops thick, wart-like scales. This condition is caused by mutations in genes responsible for producing keratin, a protein essential for skin strength and integrity. Individuals with Epidermolytic Ichthyosis require careful management to prevent infections and manage discomfort.
Causes of Ichthyosis
The root causes of ichthyosis vary depending on the specific type. However, all forms share a common feature: an abnormality in the skin’s natural shedding process, known as desquamation. Normally, the outermost layer of the skin, the stratum corneum, sheds dead skin cells regularly. In individuals with ichthyosis, this process is disrupted, leading to the accumulation of dry, scaly skin.
Genetic Factors
Most forms of ichthyosis are genetic, meaning they are passed down from parents to their children. Mutations in specific genes disrupt the production of proteins necessary for maintaining healthy skin. For example, Ichthyosis Vulgaris is linked to mutations in the filaggrin gene, which is vital for skin hydration. Similarly, X-Linked Ichthyosis is caused by a mutation in the gene responsible for producing steroid sulfatase.
Acquired Ichthyosis
In contrast to genetic forms, Acquired Ichthyosis develops later in life and is often associated with underlying medical conditions. Common triggers include kidney failure, thyroid disorders, certain cancers, and autoimmune diseases like HIV. In these cases, treating the underlying condition can sometimes alleviate the symptoms of ichthyosis.
Symptoms and Diagnosis
The symptoms of ichthyosis can vary widely depending on the type and severity of the condition. However, there are some common signs that healthcare providers look for when diagnosing ichthyosis.
Key Symptoms
- Persistent dryness and scaling of the skin
- Thickened skin on the palms and soles
- Redness and inflammation in affected areas
- Itching and discomfort
- In severe cases, skin fissures that may become infected
Diagnostic Process
Diagnosing ichthyosis typically involves a thorough physical examination and a review of the patient’s medical history. In some cases, a skin biopsy may be performed to examine the structure of the skin under a microscope. Genetic testing can also help identify specific mutations responsible for inherited forms of ichthyosis, providing valuable information for both patients and their families.
Treatment and Management
While there is no cure for ichthyosis, various treatments and lifestyle modifications can help manage symptoms and improve quality of life. The primary goal of treatment is to moisturize the skin, reduce scaling, and prevent complications such as infections and overheating.
Moisturizers and Emollients
Regular use of moisturizers and emollients is essential for individuals with ichthyosis. These products help hydrate the skin and soften scales, making them easier to remove. Ingredients such as urea, lactic acid, and glycerin are particularly effective in retaining moisture and improving skin texture.
Keratolytic Agents
Keratolytic agents, such as salicylic acid and alpha-hydroxy acids, work by breaking down the bonds between dead skin cells, promoting natural exfoliation. These treatments can be applied topically and are especially useful for reducing thickened, scaly patches of skin.
Bath and Skin Care Routine
A consistent bath and skin care routine can make a significant difference for individuals with ichthyosis. Soaking in lukewarm water with added oils or bath additives can help soften the skin before applying moisturizers. Gently patting the skin dry and immediately applying a thick layer of emollient helps lock in moisture.
Medical Treatments
In severe cases, oral medications such as retinoids may be prescribed to regulate skin cell production and reduce scaling. Retinoids can be highly effective but require careful monitoring due to potential side effects. Additionally, addressing any underlying medical conditions associated with Acquired Ichthyosis is crucial for symptom management.
Living with Ichthyosis
Managing ichthyosis requires a long-term commitment to skin care and self-care practices. Beyond medical treatments, individuals with ichthyosis can benefit from adopting certain lifestyle changes to enhance their well-being.
Psychological Impact
Living with visible skin conditions like ichthyosis can take a toll on mental health. Feelings of self-consciousness, anxiety, and depression are not uncommon. Seeking support from mental health professionals, joining support groups, and connecting with others who share similar experiences can provide emotional relief and foster resilience.
Diet and Hydration
Maintaining a balanced diet and staying hydrated can support overall skin health. Foods rich in omega-3 fatty acids, vitamins A, C, and E, and zinc are particularly beneficial for skin repair and hydration. Drinking plenty of water ensures that the body remains hydrated, which can help alleviate dryness.
Environmental Considerations
Environmental factors such as cold weather, low humidity, and exposure to harsh chemicals can exacerbate ichthyosis symptoms. Using a humidifier indoors, wearing protective clothing, and avoiding irritants can help minimize flare-ups and maintain skin comfort.
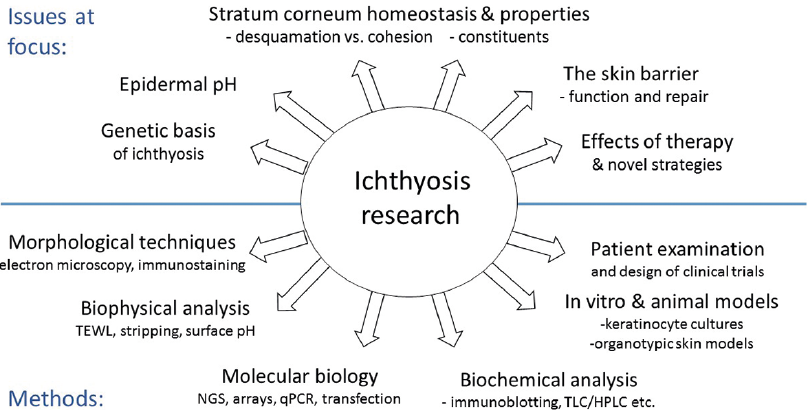
Research and Future Directions
Ongoing research into the genetic and molecular mechanisms underlying ichthyosis holds promise for developing new and more effective treatments. Advances in gene therapy, stem cell research, and personalized medicine offer hope for individuals with severe forms of the condition. By unraveling the complexities of ichthyosis, scientists aim to create targeted therapies that address the root causes rather than merely alleviating symptoms.