Hypoparathyroidism, often abbreviated as HPTH, is a rare medical condition characterized by insufficient production of parathyroid hormone. This hormone plays a critical role in regulating calcium and phosphorus levels in the body. When its levels drop, it can lead to a cascade of health issues that affect multiple systems. In this guide, we will explore everything you need to know about this condition, from its causes and symptoms to diagnosis and treatment options.
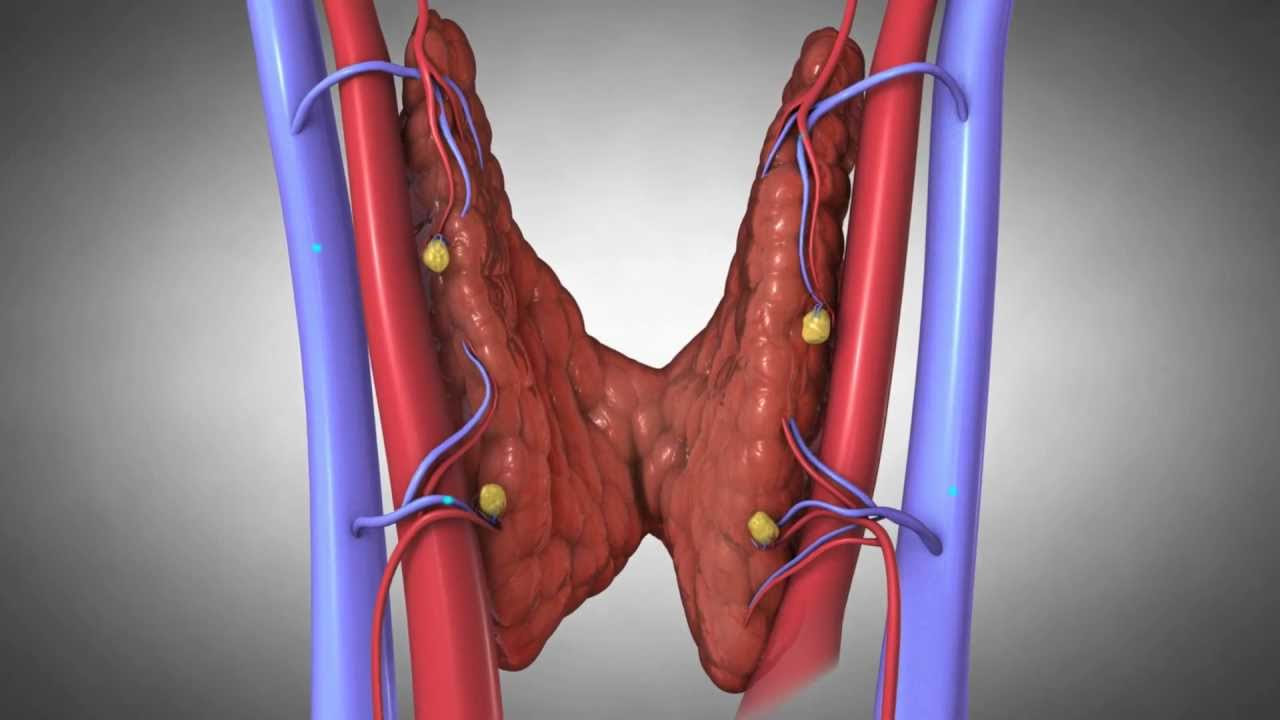
Understanding the Role of the Parathyroid Glands
The parathyroid glands are small, pea-sized structures located behind the thyroid gland in the neck. Despite their small size, these glands have a significant responsibility: they produce parathyroid hormone, which is essential for maintaining balance in the body’s calcium and phosphorus levels. Calcium is vital for muscle function, nerve transmission, and bone health, while phosphorus supports energy production and bone structure. When the parathyroid glands fail to produce enough hormone, calcium levels drop, and phosphorus levels rise, leading to a range of complications.
What Happens When Parathyroid Hormone Levels Are Low?
When the body does not produce sufficient parathyroid hormone, the delicate balance between calcium and phosphorus is disrupted. Low calcium levels, also known as hypocalcemia, can cause a variety of symptoms and complications. These may include muscle cramps, tingling sensations in the fingers and toes, fatigue, and even seizures in severe cases. Elevated phosphorus levels, on the other hand, can contribute to the formation of calcium-phosphate deposits in tissues, leading to further health problems.
Causes of Hypoparathyroidism
Hypoparathyroidism can occur due to a variety of reasons, each affecting the parathyroid glands differently. Understanding the underlying cause is crucial for effective management of the condition.
Surgical Removal or Damage to the Parathyroid Glands
One of the most common causes of this condition is surgical removal or damage to the parathyroid glands during neck surgery. This often happens during procedures involving the thyroid gland, such as thyroidectomy. Surgeons may inadvertently remove or damage the parathyroid glands, leading to reduced hormone production.
Autoimmune Disorders
In some cases, the immune system mistakenly attacks the parathyroid glands, impairing their ability to produce hormone. This autoimmune response can be part of a broader autoimmune disorder or occur independently.
Genetic Factors
- DiGeorge Syndrome: A genetic disorder that affects the development of the parathyroid glands, among other structures.
- Familial Hypoparathyroidism: A hereditary condition where individuals inherit a predisposition to low parathyroid hormone levels.
Magnesium Deficiency
Magnesium is essential for the proper functioning of the parathyroid glands. A deficiency in magnesium can impair the glands’ ability to produce hormone, resulting in low levels.
Symptoms of Hypoparathyroidism
The symptoms of this condition are primarily related to low calcium levels in the blood. These symptoms can vary in severity and may develop gradually over time.
Neuromuscular Symptoms
- Muscle cramps and spasms
- Tingling or numbness in the fingers, toes, and around the mouth
- Seizures in severe cases
Psychological Symptoms
- Irritability and mood swings
- Depression and anxiety
- Cognitive difficulties, such as memory problems
Other Symptoms
- Dry skin and brittle nails
- Hair loss
- Cataracts in the eyes
Diagnosis of Hypoparathyroidism
Diagnosing this condition involves a combination of clinical evaluation, blood tests, and imaging studies. Early and accurate diagnosis is essential for preventing complications.
Blood Tests
Blood tests are the primary tool for diagnosing this condition. Doctors measure levels of calcium, phosphorus, and parathyroid hormone in the blood. Low calcium levels, high phosphorus levels, and low or undetectable parathyroid hormone levels are indicative of the condition.
Urine Tests
Urine tests may be conducted to assess how much calcium is being excreted by the kidneys. High urinary calcium levels can provide additional evidence of the condition.
Imaging Studies
In some cases, imaging studies such as ultrasound or CT scans may be used to evaluate the structure and function of the parathyroid glands. These tests can help identify any abnormalities or damage to the glands.
Treatment Options for Hypoparathyroidism
While there is no cure for this condition, treatment focuses on managing symptoms and restoring normal calcium and phosphorus levels in the body. The goal is to alleviate symptoms and prevent long-term complications.
Calcium and Vitamin D Supplements
Oral calcium supplements are often prescribed to raise calcium levels in the blood. Vitamin D supplements, particularly active forms like calcitriol, are also used to enhance calcium absorption in the intestines. Regular monitoring of blood levels is necessary to adjust dosages and avoid complications such as kidney stones.
Thiazide Diuretics
In some cases, medications called thiazide diuretics may be prescribed to reduce calcium excretion through the kidneys. These medications can help maintain higher calcium levels in the blood.
Hormone Replacement Therapy
For individuals with severe cases, synthetic parathyroid hormone may be administered via injections. This treatment option is relatively new and is typically reserved for those who do not respond well to traditional therapies.
Lifestyle Modifications
Dietary changes can play a supportive role in managing this condition. Consuming foods rich in calcium, such as dairy products, leafy greens, and fortified cereals, can help maintain adequate calcium levels. Avoiding foods high in phosphorus, such as processed meats and carbonated beverages, is also recommended.
Potential Complications of Hypoparathyroidism
If left untreated, this condition can lead to serious complications that affect various systems in the body. Awareness of these potential risks underscores the importance of timely diagnosis and treatment.
Bone Health Issues
Chronic low calcium levels can weaken bones, increasing the risk of fractures and osteoporosis. Over time, this can significantly impact mobility and quality of life.
Kidney Problems
High phosphorus levels and excessive calcium excretion can lead to kidney stones and impaired kidney function. This highlights the need for regular monitoring and appropriate treatment adjustments.
Neurological Complications
Prolonged hypocalcemia can result in neurological issues, including seizures, cognitive impairment, and even permanent brain damage in severe cases.
Living with Hypoparathyroidism
Managing this condition requires a proactive approach and ongoing collaboration with healthcare providers. Patients are encouraged to stay informed about their condition and actively participate in their care.
Regular Monitoring
Frequent blood tests are necessary to monitor calcium, phosphorus, and parathyroid hormone levels. Adjustments to treatment plans may be required based on these results.
Educational Resources
Patient education is a key component of managing this condition. Understanding the importance of medication adherence, dietary modifications, and recognizing symptoms of imbalance can empower individuals to take control of their health.
Support Networks
Connecting with support groups and communities of individuals living with this condition can provide emotional support and practical advice. Sharing experiences and strategies can help patients navigate the challenges of living with this chronic condition.