Hypertrophic Cardiomyopathy, commonly abbreviated as HCM, is a condition that affects the heart muscle, causing it to thicken abnormally. This thickening can interfere with the heart’s ability to pump blood effectively and may lead to serious complications. Understanding this condition, its symptoms, diagnosis methods, and care options is crucial for managing it effectively. In this article, we will explore all aspects of this disease in detail.
What is Hypertrophic Cardiomyopathy?
Hypertrophic Cardiomyopathy is a genetic disorder that causes the walls of the heart, particularly the left ventricle, to become excessively thick. This thickening can occur in different parts of the heart but most commonly affects the septum, which is the wall separating the two lower chambers of the heart. The condition can disrupt the normal flow of blood out of the heart, leading to various complications.
Causes of Hypertrophic Cardiomyopathy
The primary cause of this condition is genetic mutations that affect the proteins responsible for the structure and function of the heart muscle. These mutations are often inherited, meaning they can be passed down from parents to their children. However, in some cases, the condition may develop without any known family history.
Risk Factors
- A family history of the condition
- Presence of certain genetic mutations
- Age (it can develop at any age but is often diagnosed in young adults)
Symptoms of Hypertrophic Cardiomyopathy
One of the challenges of diagnosing this condition is that many people with it do not experience noticeable symptoms. However, when symptoms do occur, they can vary widely in severity and may include:
Common Symptoms
- Chest pain, especially during physical activity
- Shortness of breath, even with minimal exertion
- Fatigue or feeling unusually tired
- Fainting or near-fainting episodes, particularly during exercise
- Heart palpitations, or the sensation of a racing or irregular heartbeat
Less Common Symptoms
- Swelling in the legs or abdomen due to fluid buildup
- Dizziness or lightheadedness
Diagnosing Hypertrophic Cardiomyopathy
Diagnosing this condition involves a combination of medical history evaluation, physical examinations, and specialized tests. Early and accurate diagnosis is essential for effective management of the disease.
Medical History and Physical Examination
Doctors typically begin by reviewing the patient’s medical history and asking about any symptoms they may be experiencing. They will also inquire about family history, as this condition is often hereditary. During the physical examination, the doctor may listen to the heart for abnormal sounds, such as murmurs, which can indicate issues with blood flow.
Diagnostic Tests
To confirm the presence of this condition, doctors rely on several diagnostic tools:
Echocardiogram
An echocardiogram uses sound waves to create detailed images of the heart. This test helps doctors assess the thickness of the heart muscle, evaluate how well the heart is pumping, and identify any obstructions to blood flow.
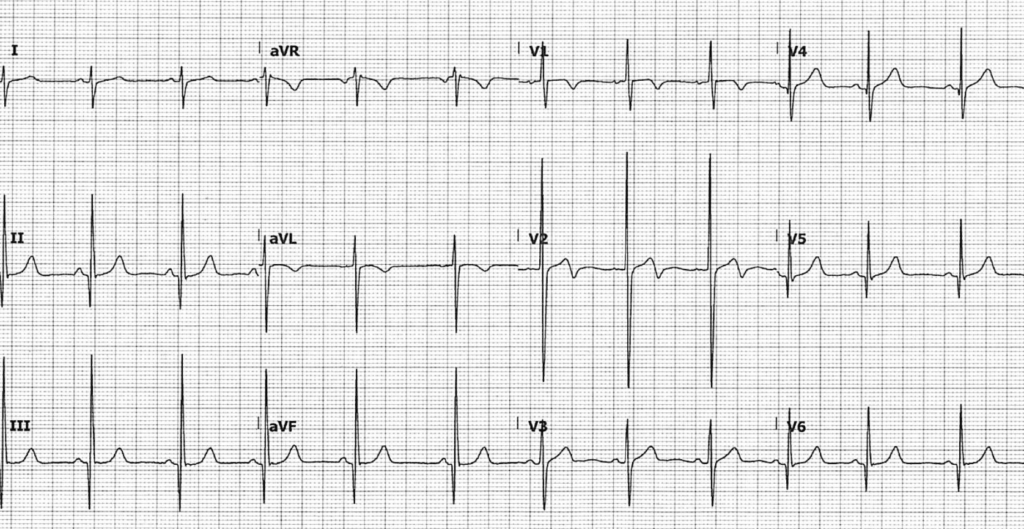
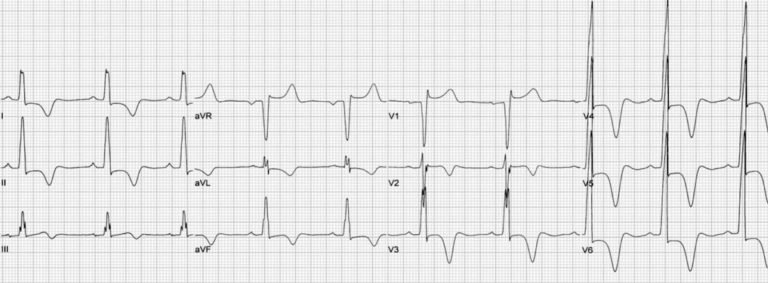
Electrocardiogram
An electrocardiogram records the electrical activity of the heart. It can detect abnormal heart rhythms and other signs that may suggest the presence of this condition.
Magnetic Resonance Imaging
Magnetic resonance imaging provides highly detailed images of the heart and can help doctors determine the extent of muscle thickening and scarring.
Genetic Testing
Since this condition is often caused by genetic mutations, genetic testing may be recommended for patients and their family members to identify whether they carry the mutation associated with the disease.
Treatment and Care Options
While there is no cure for this condition, treatment focuses on managing symptoms, preventing complications, and improving quality of life. The specific approach to care depends on the severity of the condition and the individual needs of the patient.
Lifestyle Modifications
Making certain lifestyle changes can significantly improve symptoms and reduce the risk of complications:
- Avoiding strenuous physical activities that strain the heart
- Maintaining a healthy weight to reduce stress on the heart
- Adopting a heart-healthy diet low in sodium and saturated fats
- Quitting smoking and limiting alcohol consumption
Medications
Several medications can help manage symptoms and improve heart function:
Beta-Blockers
These medications slow the heart rate and reduce the force of heart contractions, which can alleviate symptoms like chest pain and shortness of breath.
Calcium Channel Blockers
These drugs relax the heart muscle and improve blood flow, making it easier for the heart to pump blood.
Antiarrhythmic Medications
These are used to control abnormal heart rhythms and prevent complications like sudden cardiac arrest.
Procedures and Surgeries
In more severe cases, procedures or surgeries may be necessary to address complications or improve heart function:
Septal Myectomy
This surgical procedure involves removing part of the thickened heart muscle to improve blood flow and reduce symptoms.
Alcohol Septal Ablation
This minimally invasive procedure involves injecting alcohol into specific areas of the heart muscle to shrink the thickened tissue.
Implantable Devices
Devices such as pacemakers or implantable cardioverter-defibrillators may be recommended to regulate heart rhythm and prevent sudden cardiac events.
Living with Hypertrophic Cardiomyopathy
Managing this condition requires ongoing care and vigilance. Patients are encouraged to work closely with their healthcare team to monitor their condition and adjust treatment plans as needed.
Regular Monitoring
Frequent check-ups and follow-up tests are essential to track the progression of the disease and ensure that treatments remain effective. Doctors may recommend periodic echocardiograms, electrocardiograms, or other tests to assess heart function.
Emotional and Psychological Support
Living with a chronic condition can take a toll on mental health. Patients may benefit from joining support groups or seeking counseling to cope with the emotional challenges of managing the disease.
Emergency Preparedness
Patients should be aware of warning signs that require immediate medical attention, such as severe chest pain, fainting, or rapid heartbeats. Having an emergency plan in place can help ensure timely intervention in critical situations.
Preventing Complications
While some complications of this condition cannot be entirely prevented, certain measures can reduce risks:
Screening Family Members
Since this condition is often hereditary, screening family members for early signs of the disease is crucial. Early detection allows for prompt intervention and better outcomes.
Managing Comorbid Conditions
Conditions like high blood pressure, diabetes, and obesity can worsen heart health. Managing these conditions through medication, diet, and lifestyle changes is vital for reducing overall cardiovascular risk.
Staying Informed
Patients should educate themselves about their condition and stay updated on advancements in treatment options. Knowledge empowers individuals to make informed decisions about their care.