The Human Papillomavirus, commonly abbreviated as HPV, is one of the most prevalent sexually transmitted infections worldwide. It affects millions of individuals each year and has been linked to various health complications, including certain types of cancers. Despite its widespread nature, there remains a significant lack of awareness about this virus, its types, how it spreads, and how it can be prevented. This article aims to provide a comprehensive overview of the infection, detailing its characteristics, transmission methods, and preventive measures.
Understanding the Virus
Human Papillomavirus is a group of more than 200 related viruses, each identified by a specific number. These viruses are classified into two main categories based on their potential to cause cancer: low-risk and high-risk types. The low-risk types are generally associated with benign conditions such as warts, while the high-risk types have been linked to more severe health issues, including cervical cancer and other malignancies.
The virus primarily infects the skin and mucous membranes, making areas such as the genitals, mouth, and throat susceptible to infection. Its ability to remain asymptomatic in many cases makes it particularly challenging to detect without proper screening.
Low-Risk Types
- Type 6 and Type 11: These are among the most common low-risk types, responsible for approximately 90 percent of genital warts. While these warts may cause discomfort or embarrassment, they do not lead to cancer.
- Other Low-Risk Variants: There are several other low-risk types that can cause warts on different parts of the body, such as the hands and feet. These variants are generally harmless but can be persistent if left untreated.
High-Risk Types
- Type 16 and Type 18: These two types are responsible for the majority of HPV-related cancers, including cervical, anal, and oropharyngeal cancers. They account for approximately 70 percent of cervical cancer cases globally.
- Other High-Risk Variants: Additional high-risk types include 31, 33, 45, 52, and 58, which collectively contribute to a significant proportion of cancer diagnoses linked to the virus.
How the Virus Spreads
The primary mode of transmission for this virus is through intimate skin-to-skin contact, most commonly during sexual activity. However, it is important to note that the virus can also spread through non-sexual means, albeit less frequently.
Sexual Transmission
- Vaginal and Anal Intercourse: Engaging in unprotected vaginal or anal sex significantly increases the risk of contracting the virus. Even individuals who have had only one sexual partner can become infected.
- Oral Sex: The virus can also be transmitted through oral sex, leading to infections in the mouth and throat. This mode of transmission has been linked to an increase in oropharyngeal cancers.
- Skin-to-Skin Contact: Unlike many other sexually transmitted infections, penetration is not necessary for transmission. Any direct contact with infected skin or mucous membranes can result in the spread of the virus.
Non-Sexual Transmission
- Mother-to-Child Transmission: In rare cases, the virus can be passed from an infected mother to her baby during childbirth. This can lead to a condition known as recurrent respiratory papillomatosis, where warts develop in the child’s throat.
- Fomite Transmission: Although uncommon, the virus can potentially spread through contaminated objects such as towels or clothing, especially if there is direct contact with infected skin or bodily fluids.
Risk Factors for Infection
Certain factors can increase an individual’s likelihood of contracting the virus. Understanding these risk factors is crucial for taking preventive measures.
Number of Sexual Partners
Having multiple sexual partners or engaging in sexual activity with someone who has had multiple partners increases the risk of exposure to the virus. This is because the probability of encountering an infected individual rises with the number of partners.
Weakened Immune System
Individuals with weakened immune systems, such as those living with HIV or undergoing immunosuppressive treatments, are more susceptible to infection. A compromised immune system may struggle to clear the virus, increasing the likelihood of persistent infection and associated complications.
Age and Gender
Younger individuals, particularly those in their late teens and early twenties, are at a higher risk due to increased sexual activity and lower immunity against the virus. Additionally, women are disproportionately affected by certain high-risk types, as they are more likely to develop cervical cancer as a result of persistent infection.
Preventive Measures
While there is no cure for the virus once contracted, several strategies can help prevent infection and reduce the risk of complications.
Vaccination
One of the most effective ways to prevent infection is through vaccination. Vaccines are available that target the most common low-risk and high-risk types of the virus. These vaccines are typically administered during adolescence, before individuals become sexually active, to ensure maximum protection.
- Recommended Age for Vaccination: The vaccine is most effective when given between the ages of 9 and 14, although it can still provide benefits to older individuals who have not yet been exposed to the virus.
- Types of Vaccines: Different vaccines are designed to protect against varying numbers of virus types. For example, some vaccines target only two high-risk types, while others offer broader protection against nine types.
Safe Sexual Practices
Practicing safe sex is another critical preventive measure. While condoms do not provide complete protection against the virus due to its ability to infect areas not covered by the condom, they can significantly reduce the risk of transmission.
- Consistent Condom Use: Using condoms consistently and correctly during every sexual encounter can lower the chances of contracting the virus.
- Limiting Sexual Partners: Reducing the number of sexual partners and maintaining mutual monogamy with an uninfected partner can further decrease the risk of exposure.
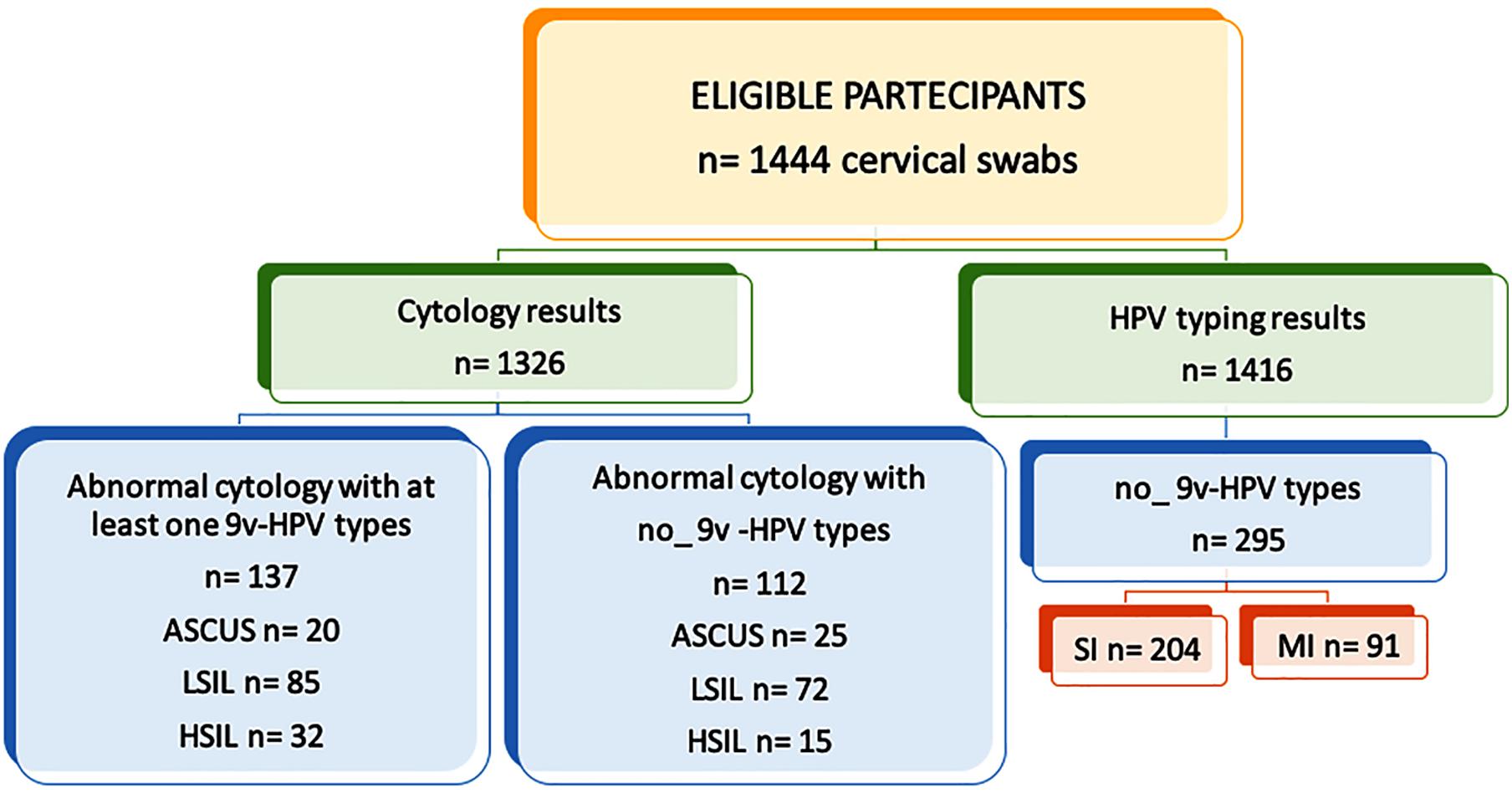
Regular Screening
For women, regular screening through Pap smears and HPV tests is essential for early detection of abnormalities caused by high-risk types. Early identification allows for timely intervention and treatment, reducing the risk of progression to cancer.
- Pap Smear: This test involves collecting cells from the cervix to check for precancerous changes caused by the virus.
- HPV Test: This test specifically detects the presence of high-risk types in cervical cells, providing additional information to guide treatment decisions.
Healthy Lifestyle Choices
Maintaining a strong immune system can help the body clear the virus naturally. Adopting healthy lifestyle choices, such as eating a balanced diet, exercising regularly, and avoiding smoking, can support overall immune function.
- Diet and Nutrition: Consuming a diet rich in fruits, vegetables, and antioxidants can boost the immune system’s ability to fight off infections.
- Avoiding Smoking: Smoking weakens the immune system and has been shown to increase the risk of persistent infection and cancer development.
Addressing Misconceptions
There are several misconceptions surrounding the virus that can hinder prevention efforts. Addressing these myths is essential for promoting accurate information and encouraging proactive behavior.
Myth: Only Promiscuous Individuals Get Infected
This is a common misconception that stigmatizes those affected by the virus. In reality, anyone who is sexually active is at risk, regardless of their number of partners. Even individuals in long-term, monogamous relationships can contract the virus if their partner was previously exposed.
Myth: Vaccination Is Only for Women
While the virus is often associated with cervical cancer in women, men are also at risk of developing cancers and transmitting the virus to their partners. Vaccination is equally important for both genders to ensure comprehensive protection.
Myth: The Virus Always Causes Symptoms
Many people believe that the virus will always present noticeable symptoms, such as warts. However, the majority of infections are asymptomatic, making regular screening and vaccination even more critical for early detection and prevention.