Histoplasmosis, often abbreviated as Histo, is a fungal infection that primarily affects the lungs. This condition arises when individuals inhale spores of a fungus commonly found in soil and bird or bat droppings. While many people who contract this infection experience mild or no symptoms, it can become severe, especially for those with weakened immune systems. Understanding the causes, recognizing the symptoms, and knowing how to manage and care for this condition are essential steps in preventing complications.
What Causes Histoplasmosis?
The primary cause of histoplasmosis is exposure to a fungus known as Histoplasma capsulatum. This fungus thrives in environments rich in organic material, particularly soil contaminated with bird or bat droppings. Here are some common sources of exposure:
- Construction sites where soil is disturbed
- Caves inhabited by bats
- Chicken coops or areas with large populations of birds
- Old buildings with accumulated bird droppings
When the soil containing the fungus is disturbed, microscopic spores are released into the air. These spores can then be inhaled, leading to infection. People who work in agriculture, construction, or other professions that involve frequent contact with soil or enclosed spaces are at a higher risk of exposure.
How Does the Infection Develop?
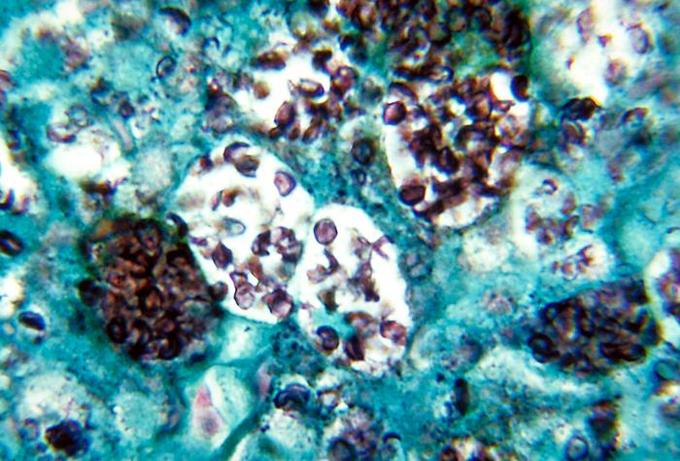
Once inhaled, the spores travel to the lungs, where they begin to grow. In healthy individuals, the immune system typically contains the infection, preventing it from spreading. However, in individuals with compromised immune systems, such as those living with HIV/AIDS or undergoing chemotherapy, the infection can spread beyond the lungs to other parts of the body, including the liver, spleen, and bone marrow.
Symptoms of Histoplasmosis
The symptoms of histoplasmosis vary depending on the severity of the infection and the individual’s immune response. Many people who contract the infection may not experience any noticeable symptoms, while others may develop mild flu-like symptoms. In more severe cases, the infection can lead to chronic lung disease or systemic illness.
Mild Cases
In mild cases, the symptoms of histoplasmosis may include:
- Fever
- Chills
- Muscle aches
- Cough
- Fatigue
- Chest discomfort
These symptoms usually appear within three to seventeen days after exposure and resolve on their own without medical intervention. Most people recover fully without realizing they had the infection.
Severe Cases
In individuals with weakened immune systems or pre-existing lung conditions, histoplasmosis can progress to a more severe form. Symptoms of severe histoplasmosis may include:
- High fever
- Shortness of breath
- Weight loss
- Night sweats
- Persistent cough with blood-tinged sputum
If left untreated, severe histoplasmosis can lead to complications such as chronic pulmonary histoplasmosis, which resembles tuberculosis, or disseminated histoplasmosis, where the infection spreads to multiple organs.
Risk Factors for Histoplasmosis
While anyone can contract histoplasmosis, certain factors increase the likelihood of developing the infection or experiencing severe symptoms. These include:
- Living or working in areas where the fungus is prevalent, such as the Ohio and Mississippi River valleys in the United States
- Having a weakened immune system due to conditions like HIV/AIDS, diabetes, or cancer
- Engaging in activities that disturb soil, such as farming, construction, or spelunking
- Being an infant or elderly, as these age groups have less robust immune defenses
Diagnosing Histoplasmosis
Diagnosing histoplasmosis can be challenging because its symptoms mimic those of other respiratory infections. Healthcare providers rely on a combination of patient history, physical examination, and diagnostic tests to confirm the presence of the infection.
Common Diagnostic Methods
To diagnose histoplasmosis, doctors may use the following methods:
- Blood Tests: These detect antibodies or antigens produced by the immune system in response to the fungus.
- Urine Tests: A urine sample can be analyzed for the presence of specific fungal antigens.
- Chest X-rays or CT Scans: Imaging tests help identify abnormalities in the lungs, such as nodules or scarring.
- Sputum Culture: A sample of mucus from the lungs is cultured in a lab to identify the fungus.
Early and accurate diagnosis is crucial for effective treatment, especially in individuals with weakened immune systems.
Treatment Options for Histoplasmosis
Treatment for histoplasmosis depends on the severity of the infection and the overall health of the individual. In mild cases, treatment may not be necessary, as the immune system can clear the infection on its own. However, for moderate to severe cases, antifungal medications are prescribed.
Antifungal Medications
The most commonly used antifungal drugs for treating histoplasmosis include:
- Itraconazole: Often used for mild to moderate cases
- Amphotericin B: Reserved for severe or disseminated infections
Patients with chronic or disseminated histoplasmosis may require long-term treatment, sometimes lasting several months to a year. It is essential to follow the prescribed treatment plan and attend regular follow-up appointments to monitor progress.
Supportive Care
In addition to antifungal medications, supportive care measures can help alleviate symptoms and improve recovery. These may include:
- Oxygen therapy for individuals experiencing shortness of breath
- Pain relievers to manage chest discomfort or muscle aches
- Adequate rest and hydration to support the immune system
Preventing Histoplasmosis
While it may not always be possible to avoid exposure to the fungus, certain precautions can reduce the risk of contracting histoplasmosis. These preventive measures are especially important for individuals with weakened immune systems or those living in endemic areas.
Practical Prevention Tips
To minimize the risk of exposure, consider the following tips:
- Avoid disturbing soil in areas known to harbor bird or bat droppings
- Wear masks or respirators when working in environments where the fungus may be present
- Ensure proper ventilation in enclosed spaces, such as caves or old buildings
- Clean and disinfect surfaces contaminated with bird or bat droppings
For individuals with compromised immune systems, consulting a healthcare provider before traveling to endemic regions is advisable.
Caring for Someone with Histoplasmosis
If you are caring for someone diagnosed with histoplasmosis, there are several ways you can support their recovery and well-being. Providing emotional support, ensuring adherence to treatment, and monitoring for complications are key aspects of caregiving.
Tips for Caregivers
Here are some practical tips for caregivers:
- Encourage the individual to take their medications as prescribed
- Help them maintain a healthy diet to boost their immune system
- Monitor for worsening symptoms, such as difficulty breathing or persistent fever, and seek medical attention if needed
- Create a comfortable and stress-free environment to promote healing
By staying informed and proactive, caregivers can play a vital role in managing histoplasmosis and ensuring a smoother recovery process.